- LOGIN
- MemberShip
- 2025-12-18 02:39:57
- Policy
- "Regulatory hurdle eliminated to simply refund-type RSA"
- by Lee, Jeong-Hwan Mar 28, 2025 06:37am
- The government saw eliminating regulatory hurdle as a success in exempting the efficacy·cost-effectiveness evaluation procedure during the 'third-contract termination evaluation' for pharmaceuticals on the basic refund-type RSA for over 10 years. Even drugs that have been subject to fines or other administrative sanctions can still have their prices increased through negotiations with the National Health Insurance Service (NHIS) if supply shortages disrupt patient care. For example, if a pharmaceutical company that produces plasma fractionation products can prove production cost increases based on additional research into pricing models for raw plasma and related inputs, the government covers not only past losses but also future cost escalations, a policy to raise prices accordingly. This measure is regarded as a notable case of eliminating regulatory hurdle. On March 25, the government convened the 6th Bio-Health Innovation Commission at the ARPA-H Promotion Team conference room on the 16th floor of City Tower in Jung-gu, Seoul, chaired by Director Kim Young-tae, Vice Chairman from the private sector and Director of Seoul National University Hospital, to discuss improvements to so-called "killer regulations." The Ministry of Health and Welfare (MOHW) suggested several regulatory improvement initiatives, including enhancements to the repeated re-evaluation process for risk-sharing agreements, revisions to the evaluation criteria for drug price caps, and establishment of a cost-calculation methodology for plasma fractionation products. Under revised guidelines, drugs subject to a basic refund-type RSA contract that has been used for more than 10 years can exempted from the utility and cost-effectiveness assessment during the 'third-contract termination evaluation.' The MOHW believes these changes will help resolve issues such as the devaluation of new drugs due to repeated re-evaluation under risk-sharing agreements and the consequent delays in the domestic introduction of new therapies. As of January of this year, the MOHW improved the evaluation criteria so that even drugs facing administrative sanctions, such as fines, can be considered for ceiling price adjustments to enhance patient treatment access and ensure pharmaceutical access. In cases where drug supply shortages may disrupt patient care, it has become possible to negotiate with the NHIS to raise drug prices. Furthermore, the government implemented the regulatory revision to improve plasma fractionation products' stable supply and cost-effectiveness. After a decision by the Health Insurance Policy Deliberation Committee, a change has been made to the price ceiling for plasma fractionation products that are already listed. If a manufacturer can substantiate, based on additional research into pricing models for raw plasma and similar inputs, that cost-increasing factors exist, then prices may be raised not only to cover past losses but also to account for future cost escalations. The MOHW has also relaxed the criteria for accepting efficacy evidence in high-risk advanced regenerative medicine clinical trials. In order to alleviate the burden associated with such high-risk studies of advanced regenerative medicine, the 'Guidelines for Reviewing and Preparing Advanced Regenerative Medicine Clinical Trial Plans' have been revised to establish exception criteria for safety and efficacy evidence. Through these measures, institutions conducting regenerative medicine trials will be able to choose appropriate testing methods that can adequately demonstrate safety and efficacy, even if there are variations in administration routes or methods, provided that additional supporting data justifying changes in clinical design are submitted in line with the specific characteristics of each study. Monitoring implementation of Bio-Health Training Strategies An assessment of the progress of 81 bio-health training projects, managed by nine ministries in 2024, revealed that a total of 44,800 bio-health professionals have been trained. This figure far exceeds the target of 22,100 reported to the 2nd Bio-Health Innovation Commission last year. The government analyzed that this substantial increase is due to growing interest in the bio-health sector, which has led to the establishment of new courses, increased demand for education, and an expansion of educational institutions. In detail, in one of the four major areas of bio-health human resource development, such as "industry-based school education," enhanced practical training and strengthened industry-academia linkages have produced approximately 16,400 professionals. In addition, around 20,000 individuals have been trained in the area of production and regulatory science, including workforce development (through institutions like K-NIBRT), regulatory science, and continuing education for current employees. Furthermore, to support the NEXT semiconductor leap through core research human resource development, via initiatives in AI-driven drug development, specialized graduate schools, and programs for physician-scientists, about 8,000 professionals have been trained, and projects aimed at stimulating local employment and linking job creation with start-up support have also been successfully advanced. This year, in line with the plans of the various ministries, 10 of the original 81 projects that have either been completed or will not be pursued this year will be excluded, while 7 new projects will be initiated. In total, 26,900 professionals are planned to be trained across 78 projects. Additionally, the government will focus on expanding interdisciplinary education, practical talent development programs, and initiatives for training professionals in new technology sectors within school curriculum. Furthermore, the Bio-Health Innovation Commission has reviewed research findings reflecting input from industry and academic experts on the persistent mismatch between the supply and demand of bio-health professionals, and is now discussing future strategies based on these insights. The research identified the primary factors contributing to the human resource mismatch as a lack of industry input in university curriculum, a skewed focus in human resource development that leaves a gap in understanding specialized fields such as new technologies, and a shortage of expert personnel (professors and instructors). In response, the Commission agreed on the importance of cultivating professionals tailored to corporate needs, training professionals to meet future demands in new technologies, and training globally competitive expert instructors. Going forward, the government plans to publish a '2025 Bio-Health Talent Development Business Guide' in May to boost awareness and participation among job seekers, schools, and educational institutions regarding these talent development initiatives. Going forward, the government plans to publish a '2025 Bio-Health Talent Development Business Guide' in May to boost awareness and participation among job seekers, schools, and educational institutions regarding these talent development initiatives. Director Kim stated, "At today’s meeting, we were able to discuss topics on a government-wide support plan to maximize industry capabilities by reviewing the implementation status of bio-health human resource development projects and improvements in regulatory issues," adding, "We will continue to monitor these issues regularly at the level of the Bio-Health Innovation Commission and strive to ensure that today’s discussions are reflected in government policies, aimed to achieve clear outcomes."
- Policy
- Vocabria·Rekambys newly listed…expanded reimb for Xeljanz
- by Lee, Jeong-Hwan Mar 26, 2025 06:00am
- Product photos of Vocabria, Xeljanz, and FexuclueThe HIV treatments Vocabria (cabotegravir) and Rekambys (rilpivirine) will be newly added to the National Health Insurance reimbursement list next month. The scope of reimbursement will be expanded for Pfizer's autoimmune diseases treatment Xeljanz (tofacitinib), Novartis' Cosentyx (secukinumab), and Daewoong's erosive gastroesophageal reflux disease treatment Fexuclue (fexuprazan). On March 20, the Ministry of Health and Welfare (MOHW) announced this on the administrative notification board regarding the 'Draft for Partial Revision to the Criteria and Scope of National Health Insurance (Pharmaceuticals).' The revision will be implemented on April 1, and the MOHW will collect opinions until the 24th. For HIV therapies, in addition to the conventional cocktail regimen, PrEP and three products, including Vocabria Tab 30 mg, Vocabria injections, and Rekambys injections, have been added to the National Health Insurance reimbursement list. Reimbursement is applicable only when the drugs are administered within the approved indications. The ceiling prices for Vocabria Tab 30 mg is KRW 16,303 per tablet, for Vocabria injections is KRW 991,802 per vial, and for Rekambys injections is KRW 434,550 per vial. The National Health Insurance reimbursement criteria will be added to oral tofacitinib, such as Xeljanz, to include juvenile idiopathic arthritis. Oral tofacitinib can be used to treat children (age 2 to 17) diagnosed with juvenile idiopathic arthritis according to the ILAR criteria (2001 revision), including ▲Polyarticular arthritis that affects five or more joints ▲Extended oligoarthritis ▲Psoriatic arthritis ▲Those who discontinued treatments due to inadequate response to one or more biological agent or side effects. After 6 months of usage, an additional 6-month usage will be approved if an assessment indicates a decrease of over 30% in the number of inflammatory joints compared to the initial administration timepoint. After that, the evaluation will be carried out every 6 months, and when the assessment result in the first 6 months is maintained, consistent administration will be approved. If a patient diagnosed with juvenile idiopathic arthritis before age 17, beyond the scope, subsequently uses a medication that meets the reimbursement criteria after turning 17, reimbursement will be applied. Cosentyx received an expanded reimbursement scope for chronic severe plaque psoriasis, lowering the age threshold from 18 years or older to 6 years or older. For Fexuclue, the reimbursement criteria for the 10 mg oral formulation has been updated to include "improvement of gastric mucosal lesions in acute and chronic gastritis." Additionally, for orally administered triple combination therapy for antidiabetic medications, 'triple combination therapy containing dapagliflozin+sitagliptin+metformin' has been added to reimbursed ingredients of an SGLT‑2 inhibitor, a DPP‑4 inhibitor or a biguanide product. Furthermore, the reimbursement criteria for the ENT product Ryaltris Nasal Spray Sol (olopatadine+mometasone furoate) will be expanded due to changes in its MFDS-approved labeling. Although the previous approval limited its use to patients aged 12 and older, the age range has now been extended to 6 years and above. Consequently, reimbursement is granted only for seasonal allergic rhinitis in adults and adolescents aged 12 or older, while children aged 6 to 11 will cost 100% copay. As the inclusion of the gastrointestinal drug Irricol Tab to the listing is anticipated, the existing oral product Irribow Tab (ramosetron HCl 2.5 μg and 5 μg) has been added to the reimbursement criteria.
- Policy
- New law proposed for the cancer and rare disease fund
- by Lee, Jeong-Hwan Mar 25, 2025 05:54am
- A bill to establish a new fund for cancer and rare diseases to strengthen patient access to ultra-high-priced drugs has been proposed to the National Assembly. The fund will be raised through transfers and deposits from other funds, such as the lottery fund. On the 24th, National Assembly member Myeong-ok Seo (People Power Party), a member of the National Assembly's Health and Welfare Committee, announced that she had submitted a bill to establish the Cancer Management Fund and the Rare Disease Management Fund. The main points of the bill include ▲the establishment of a cancer management fund for the prevention and treatment of cancer (amendment to the Cancer Management Act), ▲the establishment of a rare disease fund for the prevention and treatment of rare diseases (amendment to the Rare Disease Management Act), ▲the establishment of a basis for the establishment of the fund in the National Finance Act (amendment to the National Finance Act), and ▲the establishment of grounds for the use of the lottery fund (amendment to the Lottery Tickets and Lottery Fund Act). According to the data that Rep. Seo received from the Health Insurance Review and Assessment Service, it took an average of 332 days for an anticancer drug to be listed for reimbursement in Korea from 2014 to 2024. In particular, in the case of anticancer drugs for blood cancer and lung cancer, there were cases where it took 600 to 800 days to listing. To address this, the UK operates an anticancer drug fund and a rare drug fund. Italy also has a rare disease drug fund that is financed with 5% pharmaceutical sales promotional expenses and government funds. Although there have been attempts to establish a new cancer management fund in Korea, the attempts have been frustrated by the opposition of financial authorities, with repeated calls on the need for realistic solutions to raise necessary finances. “Currently, about KRW 85 billion of the National Health Promotion Fund is being spent on cancer prevention and treatment, so it is not impossible to use it as the source of funding as it is while using a portion of the lottery proceeds, which have been increasing rapidly recently,” explained Seo. According to recent reports, lottery sales have risen by an average of KRW 450 billion per year since 2020. Next year, lottery ticket sales are expected to exceed KRW 8 trillion for the first time in history. “In a situation where it is becoming structurally difficult to apply health insurance reimbursement to treatments for patients with cancer and rare diseases, the establishment of the fund is a matter directly related to the lives of the people,” said Rep. Seo. “I hope that the bill will prompt forward-looking discussions.”
- Policy
- Tepmetko, Tevimbra granted reimbursement in Korea
- by Lee, Tak-Sun Mar 24, 2025 05:52am
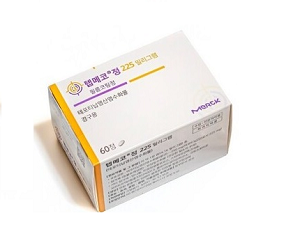
- Tepmetko Tab 225mg (tepotinib, Merck Korea). New anticancer drugs Tepmetko and Tevimbra will be included in the list of reimbursed drugs as of April 1 in Korea. In addition, the economic burden on the patients is expected to be significantly reduced as the co-insurance rate for abiraterone acetate drugs such as Zytiga has been reduced for the first-line treatment of castration-resistant prostate cancer. The Health Insurance Review & Assessment Service has announced a revision to the notice regarding the drugs prescribed and administered to cancer patients and has entered the opinion survey period. The effective date is April 1. According to the revision, Tepmetko 225 mg (tepotinib, Merck Korea) is granted reimbursement for patients with locally advanced or metastatic non-small cell lung cancer with MET exon 14 deletion. HIRA said, “We set the reimbursement criteria by considering factors such as the fact that the applied drug is a drug with a clear target and can provide patients with another treatment option, and is a drug deemed necessary for medical treatment.” Tepmetko is the only MET-mutated anticancer drug that is covered by the National Health Insurance in Korea. According to the diagnosis of 1,020 patients with non-small cell lung cancer in Korea, 1.9% of patients were confirmed to have MET exon 14 deletion. In Phase II clinical trial which added a confirmatory test arm, Tepmetko showed an ORR of 51.4% (95% CI, 45.8-57.1), mPFS of 11.2 months (95% CI, 9.5-13.8), and mOS of 19.6 months (95% CI, 16.2-22.9), confirming its high therapeutic effect. This drug is recommended in major textbooks and guidelines of overseas academic societies. The insurance ceiling price of Tepmetko is reportedly KRW 76,500 per dose. It has signed a refund-type and expenditure cap-type Risk Sharing Agreement (RSA) to share the drug’s financial burden. Tevimbra Inj (tislelizumab, BeiGene Korea) is indicated as a monotherapy for patients with unresectable, relapsed, locally advanced, or metastatic oesophageal squamous cell carcinoma who are unable to continue platinum-based chemotherapy or who have relapsed or progressed within 6 months after receiving prior platinum-based chemotherapy. However, reimbursement is granted for patients who have not received treatment with an immune checkpoint inhibitor such as a PD-1 inhibitor. As an immuno-oncology drug that has a PD-1 inhibitory mechanism of action, its reimbursement listing in April will allow the drug to become the first immuno-oncology drug to be covered for esophageal cancer in Korea. The maximum amount of this drug is KRW 1,206,000 per bottle. Like Tepmetko, it is applied the refund type and expenditure cap type RSA. Meanwhile, the co-insurance rate for abiraterone acetate formulations such as Zytiga will be reduced from 30% to 5% for the first-line treatment of castration-resistant prostate cancer. Abiraterone is available not only as the original Zytiga (Janssen Korea) but also as generic versions supplied by Hanmi Pharmaceutical and Ace Pharmaceutical. This reduction in the co-insurance rate is also related to the entry of generics. The National Health Insurance Service said, “The reimbursement of the ‘next-generation hormone drug (all-trans retinoic acid, ATRA)’ for metastatic hormone-sensitive prostate cancer will gradually decrease the number of patients eligible for this treatment. The price of the drug has been reduced upon the listing of generics, etc, and the coinsurance rate for ‘abiraterone acetate + prednisolone’ as a first-line treatment for castration-resistant prostate cancer will be reduced from 30% to 5%." The ATRA-class next-generation hormone drug is Janssen's Erleada. Erleada was listed for reimbursement in April 2023.
- Policy
- How Tevimbra was reimbursed in Korea first
- by Lee, Tak-Sun Mar 24, 2025 05:52am
- BeiGene Korea's Tevimbra will be reimbursed in Korea from next month as a second-line treatment for esophageal squamous cell carcinoma, a type of esophageal cancer. It is the first immuno-oncology drug to be covered for esophageal cancer. In particular, the drug is drawing attention as it was covered in South Korea before the A8 countries (the United States, the United Kingdom, Germany, France, Italy, Switzerland, and Japan) known as the government’s reference countries for reimbursement coverage. The reason why the drug received prompt reimbursement in Korea is that the insurance authorities have taken into account Korea’s situation, where the prevalence of esophageal cancer is relatively higher than in other countries, and that the pharmaceutical company, BeiGene Korea, also presented a reasonable drug price. According to industry sources on the 21st, Tevimbra (tislelizumab, BeiGene Korea) will be reimbursed starting next month for unresectable, recurrent, locally advanced, or metastatic esophageal squamous cell carcinoma that has relapsed or progressed during or after previous platinum-based chemotherapy. It is the first PD-1 inhibitor-based immuno-oncology drug to be covered by the National Health Insurance for esophageal cancer. Squamous cell carcinoma accounts for the largest proportion of esophageal cancer, accounting for 91% of esophageal cancer cases. In particular, its prevalence is reportedly higher in East Asia compared to that in North American and European countries. Its prognosis is also poor. Most cases are detected when the disease has progressed to a significant degree, so the survival rate is not high. According to data from the Korea Central Cancer Registry, the 5-year relative survival rate for esophageal cancer from 2017 and 2021 was only 42.8%. Platinum-based chemotherapy is mostly used as the first-line treatment for esophageal cancer, and docetaxel is used as the second-line or later treatment. Compared to existing anticancer drugs, immuno-oncology drugs have shown significant improvements in overall survival but are not widely used because they are not reimbursed by the National Health Insurance. Due to this situation, the health authorities reportedly have given high scores for Tevimbra in terms of its clinical utility. Experts at the Drug Reimbursement Evaluation Committee said, “Compared to the chemotherapy group, Tevimbra showed a significant improvement in overall survival and is safer with a lower risk of side effects than chemotherapy. Currently, there are no immuno-oncology drugs reimbursed for esophageal squamous cell carcinoma in Korea, and due to the many limitations in treatment options, Tevimbra’s introduction is necessary.” Such expert opinions were heavily reflected in the review of the drug's adequacy of reimbursement. “The fact that the number of esophageal cancer patients in Korea is higher than in the US and Europe and that the prognosis is poor was taken into consideration,” said a HIRA official. “It was difficult to assess the drug because it was not listed for reimbursement in the A8 countries and was not mentioned in major reference textbooks, but the review was conducted with a focus on the drug’s clinical aspects.” Of course, there were results from clinical studies that showed significant improvements in overall survival and progression-free survival, but there were relatively few references to textbooks or other such materials. However, there was a clinical practice guideline - the NCCN guidelines in the United States – which recommended the drug as a second-line or higher monotherapy. The company’s proposal of a reasonable drug price was also granted for the drug’s prompt reimbursement. BeiGene Korea was recognized for its cost-effectiveness by submitting the results of a pharmacoeconomic evaluation compared to docetaxel and the results of a cost-utility analysis using RSA plans (refund and expenditure cap type). BeiGene Korea has announced that it will offer a low drug price to ensure the rapid supply of Tebipembrolizumab. It is reported that the drug will be supplied at a 10% discount from existing treatments in the United States. Currently, the only immuno-oncology drugs that are undergoing the reimbursement process for esophageal cancer are Keytruda and Opdivo. They have been approved as first-line treatments, not second-line treatments. However, unlike these drugs, Tevimbra has the advantage of being able to be used regardless of PD-L1 expression. Tevimbra is an anticancer drug developed in China in 2019. The domestic approval was granted in November 2023, and the drug was successfully listed for reimbursement in 1 year and 4 months. Its price is KRW 1,206,000 per bottle, and it is expected to cost about KRW 9.65 million per year. If the 5% co-insurance rate is applied, the annual drug cost for the patients will be reduced to about KRW 480,000, which is a relatively low price for an immuno-oncology drug.
- Policy
- Enhertu’s reimb may be extended to gastric cancer
- by Lee, Tak-Sun Mar 21, 2025 05:59am
- The number of patients who can use the new antibody-drug conjugate (ADC) anticancer drug ‘Enhertu Inj (trastuzumab deruxtecan, Daiichi Sankyo Korea), which has been reimbursed since April last year, is expected to be expanded to cover eligible gastric cancer patients. This is an expansion in the scope of existing patients eligible for reimbursement. The Health Insurance Review and Assessment Service's Cancer Disease Deliberation Committee voted on the 19th to expand the reimbursement coverage of Enhertu. Enhertu is a next-generation ADC that combines a monoclonal antibody with the same structure as trastuzumab, which binds to a specific target receptor overexpressed on the surface of cancer cells, and a topoisomerase I inhibitor payload with a tumor-selective cleavable linker, which is a novel and highly potent mechanism of action. The drug is expected to have a higher therapeutic effect than existing anticancer drugs. The drug was added for reimbursement in April last year by applying a flexible incremental cost-effectiveness ratio (ICER) threshold, an indicator of economic efficiency. As a result, the patient's burden from annual medication costs was reduced from KRW 80 million to KRW 4 million. At the time, the reimbursement standard for gastric cancer patients was set as locally advanced or metastatic gastric adenocarcinoma or adenocarcinoma of the gastroesophageal junction that satisfies all three conditions. The conditions were: patients who ①failed two or more prior therapies, including trastuzumab (Herceptin) +(fluorouracil or capecitabine)+cisplatin; ②have HER2 overexpression (IHC 3+ or 'IHC 2+ and FISH+ or SISH+’) metastatic gastric adenocarcinoma or gastroesophageal junction adenocarcinoma; and ③have an ECOG performance status (PS) of 0 or 1. This expansion of the reimbursement standard this time will extend the scope of the drugs limited to cisplatin in the first condition to other platinum-based anticancer drugs. As a result, it is expected that not only cisplatin but also patients with gastric cancer who have failed to receive oxaliplatin (original Eloxatin) will be able to receive Enhertu with reimbursement. “Enhertu’s reimbursement expansion agenda extends the conditions limited to cisplatin among platinum-based anticancer drugs in the existing reimbursement standards to other platinum-based anticancer drugs,” said a HIRA official. “This is expected to further expand patient access.” The applications for which the reimbursement standards have been established at this meeting will be reviewed by the Drug Reimbursement Evaluation Committee to determine their reimbursement adequacy.
- Policy
- Public-private meetings on improving drug pricing system
- by Lee, Tak-Sun Mar 20, 2025 06:00am
- Attention has been gathered to recent public-private meetings regarding improving drug pricing system. This month, a public-private discussion session hosted by the Ministry of Health and Welfare (MOHW) and a meeting to discuss the negotiation system for expanded use of scope were held. On March 26, a regular meeting session was attended by three pharmaceutical organizations, including the National Health Insurance Service (NHIS), the Democratic Party of Korea's Future Economic Growth Strategy Committee, the Korean Research-Based Pharma Industry Association (KRPIA), and the Korea Biomedicine Industry Association (KoBIA), is scheduled. The public-private meeting was temporarily discontinued last year and resumed in February. It has been reported that two sessions have been held this year to discuss the agenda for improving the drug pricing system. The public-private meetings are attended by government agencies, such as the MOHW, NHIS, and Health Insurance Review and Assessment Service (HIRA), and three pharmaceutical organizations. As the agenda for 'incentivizing new drugs with innovative values' has been established through the public-private body in 2023, attention has been gathered to the outcome of the discussion on the drug pricing system through the upcoming meeting. The industry is expected to recommend pricing drugs based on specific indications. The organization for the negotiations system for expanded scope of use announced establishing guidelines for priority negotiations this year. Improving the negotiation system for expanded scope of use is based on the research outcome of the research initiated by the NHIS (Professor Euna Han's research team in the College of Pharmacy at Yonsei University) last year. However, the MOHW and the industry have decided to establish negotiation guidelines at this year's meetings rather than bringing improvements to the system itself. The focus of the regular meeting between NHIS-three pharmaceutical organizations on March 26 will be discussing improvements to the negotiations for expanded scope of use and choices of medicines and adjusted criteria based on the draft for 'incentivizing new drugs with innovative values.' The health authority said, "It is a regular meeting attended by pharmaceutical companies every three months," adding, "We plan to develop an agenda for system improvements through continued meetings." Meanwhile, the public-private meeting initiated by the MOHW to improve the system for surveying pharmaceutical prices in the market completed hearing opinions. It has been reported that the MOHW is contemplating on whether to conduct an additional session or write a draft based on gathered views to date. The industry expects the draft to be announced in the first half of the year. The research contains sensitive data, including companies subjected to the survey, so whether it will be reflected in the draft gathers attention.
- Policy
- Drug briefing on Enhertu's NSCLC reimb has been requested
- by Lee, Tak-Sun Mar 19, 2025 06:02am
- Product photo of Enhertu It has been reported that Daiichi Sankyo, which is aiming for Enhertu (trastuzumab deruxtecan)'s expanded reimbursement for HER2-mutant non-small cell lung cancer (NSCLC), will hold a drug briefing session with the Health Insurance Review & Assessment Service (HIRA). In April 2024, Enhertu was added to the reimbursement listing in South Korea as a treatment for HER2-positive metastatic breast cancer and gastric cancer. It has garnered attention as the drug received benefits for exceeding the incremental cost-effectiveness ratio (ICER) value, an index for economic evaluation. According to industry sources on March 17, Daiichi Sankyo recently requested a drug briefing regarding Enhertu's HER2-mutant NSCLC treatment. Enhertu, an antibody-drug conjugate (ADC) jointly developed by Daiichi Sankyo and AstraZeneca, was approved by the U.S. Food and Drug Administration (FDA) in 2019. In December 2024, Daiichi Sankyo applied for insurance reimbursement of the ADC Enhertu's two additional indications. The company had applied for Enhertu's indication to treat ▲Patients with unresectable or metastatic HER2-low (IHC 1+ or IHC 2+/ISH-) breast cancer who have previously undergone systemic therapy in the metastatic setting or relapsed within 6 months of completing adjuvant chemotherapy and hormone receptor-positive (HR+) patients who have received or are unsuitable for endocrine therapy ▲Patients with unresectable or metastatic NSCLC with activated HER2 (ERBB2) mutations who have previously received systemic therapy, including platinum-based chemotherapy. Enhertu was added to the reimbursement listing as a treatment for HER2-positive metastatic breast cancer and gastric cancer in April of last year. The ceiling price of the drug was KRW 1.43 million per vial. The Ministry of Health and Welfare (MOHW) explained that after the reimbursement of Enhertu, "Patients with HER2-positive metastatic breast cancer who spent approximately KRW 83 million annually for administration cost will now only pay KRW 4.17 million with the health insurance coverage." It has been reported that the health authority offered benefits for Enhertu's inclusion in the reimbursement list, considering the ICER value. Enhertu reportedly generated sales of approximately KRW 20 billion last year. Analysis suggests that if the reimbursement is applied to NSCLC with many patients, reimbursement claim amount will increase. As a result, whether the reimbursement will be expanded will depend on pharmaceutical company's share of financial burden. However, expanded reimbursement of Enhertu is expected to provide significant therapeutic benefits for patients, given that Enhertu has demonstrated clear efficacy. Enhertu demonstrated an anti-tumor response for the second-line treatment of HER2-mutant metastatic NSCLC through the DESTINY-Lung02 study. The clinical results demonstrated that Enhertu had Blinded Independent Central Review (BICR)-assessed confirmed ORR of 49%, complete response (CR) of 1%, and partial response (PR) of 48%. Daiichi Sankyo is expected to present these efficacy data to persuade reviewers at the HIRA. The drug briefing session was introduced in 2010 to enhance transparency and objectivity in evaluations by facilitating the mutual exchange of information about new drugs between pharmaceutical companies and evaluators. These sessions are typically held within 1-2 months after a drug evaluation application is submitted. If additional data are requested, the session is scheduled once the supplementary materials are reviewed. Attendees include HIRA personnel and related deputy directors responsible for setting the standards and reimbursement evaluations for new drugs. Daiichi Sankyo previously utilized a drug briefing session during the initial listing of Enhertu, which reportedly positively impacted its reimbursement approval, leading them to apply for another session. "Drug briefing sessions provide accurate drug information and, through two-way communication, allow for sharing any supplemental details, which can help expedite the reimbursement review process," said an industry employee.
- Policy
- Five drugs all pass DREC's reimb review in February
- by Lee, Tak-Sun Mar 17, 2025 05:59am
- All five products, including new drugs and drugs that sought expanded indications, which were reviewed by the Health Insurance Review and Assessment Service's Drug Reimbursement Evaluation Committee in February, have passed review and will be negotiating the drug’s price with the National Health Insurance Service. Drugs that are subject to conditions of acceptance below the evaluated amount are also moving on to the negotiation process and are awaiting reimbursement. According to industry sources on the 14th, the National Health Insurance Service updated its negotiation subjects to include 5 drugs - Trodelvy Inj (sacituzumab govitecan-hziy), Cabometyx Tab (cabozantinib), Ebglyss Autoinjector Inj (lebrikizumab), Adempas Tab (riociguat), and Bimzelx Autoinjector Inj (bimekizumab). These five drugs are new drugs and drugs with expanded indications that were deliberated at the 2nd Drug Reimbursement Evaluation Committee meeting held on February 6. At the DREC meeting, Adempas Tab (for pulmonary arterial hypertension only) and Trodelvy Inj (for triple-negative breast cancer) were recognized as adequate for reimbursement. As such, drug pricing negotiations were expected. However, as new drugs such as Bimzelx (psoriasis) and Ebglyss (atopic dermatitis), and Cabometyx, which has applied for an expansion of its indication to clear cell renal cell carcinoma, will only be deemed adequate for reimbursement when the companies accept an amount below the evaluated amount, their negotiation results were expected to be unclear. This is because these companies must accept the evaluation amount set by DREC or below (less than the weighted average price of the alternative drug) for negotiations to proceed. For products that accept the results of the DREC deliberation, the Ministry of Health and Welfare will issue a negotiation order to proceed with negotiations with the NHIS on drug prices and expected claims amount. Accordingly, the 3 products that received conditional approval from DREC would have accepted DREC’s deliberation results to proceed with the pricing negotiations. In the case of Ebglyss, a drug for atopic dermatitis, it accepted a price below that of competing products such as Dupixent and Adtralza. Bimzelx, a psoriasis treatment, is also expected to cost less than Stelara or Cosentyx. The negotiation period is 60 days. Negotiations are expected to be completed before the Ministry of Health and Welfare's Health Insurance Policy Deliberation Committee (HIPDC) meeting in May, so it is expected that some of the drugs will be reimbursed as early as June 1. All three drugs, Tepmetko Tab and Vocabria Tab+ Vocabria Inj+ Rekambys inj, which passed DREC review in December last year and proceeded with drug price negotiations, have completed negotiations with the NHIS are likely to be reviewed by HIPDC this month.
- Policy
- Mandatory reporting of market supply suspended drugs
- by Lee, Hye-Kyung Mar 13, 2025 05:58am
- The mandatory reporting is being considered to include drug products of suspended production·importation and supply, and 'supply shortage drugs' of which supply has been halted for more than 1 month. The Ministry of Food and Drug Safety (MFDS; Minister, Yu-Kyoung Oh) stated that it would announce on March 11 an administrative notice of revision to the 'Regulation on Notification of Production·Importation·Supply suspended drug products' and will receive opinions until March 31. The regulation concerns the notification criteria for pharmaceutical companies reporting a supply shortage of drug products. The revision details include reducing the time for reporting the discontinuance of production, importation, and supply of drug products from 60 days in advance to 180 days in advance, and it establishes a new duty to report on production and importation shortage. The MFDS has established criteria for production·importation shortage to address the issue of lack of definition of drugs sold out and drugs in supply shortage. Revision (draft) to the According to the MFDS' criteria for reporting drug supply shortages due to reduced production·importation, two types have been set as ▲A decrease in production·import volume to less than half of the three-year annual average over the next one year ▲A decrease in supply or supply suspension, including a temporary halt in production·imports for at least three months or a market supply suspension for more than one month. In the case of supply reduction, if production or imports are expected to decrease to 50% or less of the three-year annual average for the upcoming one year as of the end of each quarter, a report must be submitted to the MFDS within one month of the quarter's end. Suppose production or imports are expected to be suspended for more than three months, and market supply is expected to be halted for over one month. In that case, a supply reduction plan must be established and reported within one month. However, if the temporary suspension of production·imports·supply is extended and meets the reporting criteria, the revised plan must be reported within 10 days of the change. Supply reduction and temporary supply suspension are excluded from reporting requirements in cases where ▲Temporary suspension or reduction of production·import occurs before the designation of a reportable item ▲Temporary suspension or reduction occurs naturally due to decreased market demand, or only specific packaging units are affected without significant disruption to the overall drug supply ▲Manufacturing·import·sales suspensions resulting from administrative sanctions. Additionally, reporting on temporary supply suspensions is exempt ▲If the product has been on the market for less than three years after approval or has been produced·imported two or fewer times in the past three years ▲If the company holds inventory equivalent to its quarterly production or import volume for the past year and faces no difficulty in market supply. Additionally, as previously announced by the MFDS, the revised regulations now require companies to report supply discontinuation 180 days in advance, moving up the reporting timeline from the previous 60 days. For permanent·temporary discontinuation of drug production·import·supply due to reasons such as withdrawal of product approval or contract termination, companies must report at least 180 days before the scheduled discontinuation date. Along with enhanced reporting duty, administrative penalties have also been revised. If a company reports supply discontinuation between 180 days before the discontinuation date and the actual discontinuation date, the first violation will result in a 7-day suspension of manufacturing operations. A second violation will lead to a 15-day suspension, a third violation will result in a 1-month suspension, and a fourth violation will incur a 3-month suspension of manufacturing operations. Failure to report production reduction will also result in penalties. A first violation will result in a warning, a second violation will lead to a 15-day suspension, a third violation will result in a 1-month suspension, and a fourth violation will lead to a 3-month suspension of manufacturing operations.