- LOGIN
- MemberShip
- 2025-12-19 20:29:42
- Policy
- First generic version of Qudexy XR Cap is approved in KOR
- by Lee, Hye-Kyung Sep 25, 2024 05:49am
- The first generic version of the topiramate-based extended-release epilepsy treatment ‘Qudexy XR Cap’ has been approved in Korea. The Ministry of Food and Drug Safety granted marketing authorization for Intrio Biopharma’s ‘Topimed XR Tab. 50mg’ on the 23rd. Unlike ‘Qudexy XR Cap’ which is an oblong hard capsule formulation, Topimed XR Tab was developed as a circular extended-release film-coated tablet. Intrio Biopharma has been developing Topimed XR Tab since 2022. The original epilepsy drug that contains topiramate was Janssen's ‘Topamax Tab,’ but in 2014, the U.S. generic company Upsher-Smith developed and received U.S. FDA approval for Qudexy XR Cap, which is an extended-release capsule formulation that is not available with Topamax. Qudexy XR Cap is also the topiramate approved in Korea. The drug was also supplied by SK Chemicals in August 2017 and is listed on the KFDA's Green List and protected until January 2034. However, the newly approved Topimed XR Tab is likely to be released as a film-coated tablet formulation, rather than the capsule formulation that is being protected with a patent. This is because no pharmaceutical company has attempted to avoid Qudexy XR Cap’s patent. Topimed XR Tab is indicated ▲ as initial monotherapy in patients 6 years of age and older with partial-onset or primary generalized tonic-clonic seizures and ▲ as adjunctive therapy in children 2 years of age and older and adults with partial seizures, primary generalized tonic-clonic seizures, and seizures associated with Lennox-Gastaut syndrome (LGS). While existing immediate-release topiramate formulations are taken twice daily, this medication is an extended-release formulation that is absorbed into the body more slowly and can be taken once daily. Topiramate-based formulations are the most prescribed ingredient in the KRW 80 billion antiepileptic drug market with a sales volume of KRW 30 billion, and the outpatient prescription value of Qudexy XR Cap was KRW 3.5 billion based on UBIST last year. The drug has been covered through insurance reimbursement in Korea since February 2018.
- Policy
- Takeda's drug pricing negotiations see different results
- by Lee, Tak-Sun Sep 25, 2024 05:48am
- The drug pricing negotiations for ‘Ceprotin (Protein C Concentrate (Human))’ a new drug for severe congenital protein C deficiency supplied by Takeda Pharmaceuticals Korea, fell through. On the other hand, the company reached an agreement and completed negotiations to expand the reimbursement for the ovarian cancer treatment Zejula Cap. According to industry sources on the 24th, the National Health Insurance Service announced so while updating the list of drugs that have completed drug price negotiations. Ceprotin passed the NHIS’s Drug Reimbursement Evaluation Committee in June and began negotiating with the NHIS in July, which is the final step to a drug’s reimbursement in Korea. The drug was first approved in Korea in 2022 for the treatment of severe congenital protein C deficiency. Congenital protein C deficiency is a rare genetic condition that causes a fatal defect in the regulation of blood clotting due to a lack of protein C. It affects 1 in 4 million newborns. As the only treatment available, patients have been longing for its reimbursement, but the opportunity has passed this time. Therefore, it remains to be seen whether Takeda will reattempt its reimbursement in the future. Meanwhile, reimbursement for Takeda's Zejula Cap, which passed DREC review along with Ceprotin, will be expanded in October with the finalization of negotiations. Zejula is currently reimbursed for patients with BRCA mutations as maintenance therapy in the first- to second-line treatment of platinum-sensitive advanced ovarian cancer who have responded to platinum-based chemotherapy. In October, the reimbursement standards will change from ‘patients with BRCA mutations’ to ‘patients who are Homologous Recombination Deficiency (HRD) positive.’
- Policy
- Pharmbio releases first generic Revolade with reimb in OCT
- by Lee, Tak-Sun Sep 24, 2024 05:46am
- The first generic version of the immune thrombocytopenia treatment ‘Revolade (eltrombopag olamine)’ will be released into the market in October. Pharmbio Korea’s Revolade generic has succeeded in receiving reimbursement listing 1 year after its approval in Korea. The company had been delaying its launch due to the burden of patent infringement, but its recent success in avoiding the patent prompted it to launch the product in full force. According to industry sources on the 23rd, Pharmbio Korea’s Elpag Tab. 25 mg and 50 mg will be listed for reimbursement from October 1st. The items were approved in March last year. As a rare disease drug used for thrombopenia, Elpag Tab is a generic version of Novartis’s Revolade. Although Revolade's product patent has expired, 3 composition patents are listed on MFDS’s green list, making it difficult for latecomer generics to enter the market. Pharmbio Korea and SK Plasma sought to evade Revolade ‘s substance patent by filing for a passive trial to confirm the scope of the patent. The Intellectual Property Trial and Appeal Board ruled in favor of the generic companies’ claims in the first half of this year, clearing the patent hurdle. However, the patent dispute is not completely resolved as Novartis immediately filed a following suit to cancel the decision. In this situation, Pharmbio has decided to preemptively launch its product through reimbursement listing. Revolade treats immune thrombocytopenia (ITP), a type of bleeding disorder, by stimulating platelet production. ITP is an autoimmune disease in which the immune system mistakes the body’s platelets as foreign and attacks them. According to IQVIA, Revolade’s domestic sales amounted to KRW 9 billion last year. Pharmbio is challenging the original drug with a lower price. It has applied for a drug price lower than the calculated price, setting the price at KRW 22,849 for Elpag Tab 25 mg and KRW 44,405 for Elpag Tab 50 mg. This is 30% lower than the price of the original Revolade 25mg, which is priced at KRW 32,641, and Revolade 50mg at KRW 63,435. In the case of orphan drugs, the price is set at the same level as previously listed drugs. Pharmbio seems to have adopted a strategy to increase its market share through a relatively low price.
- Policy
- AZ's bispecific ab 'Rilvegostomig' vs Keytruda trial
- by Lee, Hye-Kyung Sep 20, 2024 05:51am
- A Phase 3 trial comparing a combination therapy containing 'Rilvegostomig (Trial name: AZD2936),' AstraZeneca's bispecific antibody gathering attention as the next-generation medicine, to 'Keytruda (pembrolizumab),' a type of immunotherapy drug used to treat cancer, will be conducted in South Korea. The Ministry of Food and Drug Safety (MFDS) has approved a Phase 3, randomized, double-blind, multicenter, and global ARTEMIDE-Lung03 study, evaluating Rilvegostomig or pembrolizumab in combination with platinum-based chemotherapy as first-line treatment for patients with metastatic non-squamous PD-L1-positive metastatic non-small cell lung cancer (NSCLC). Rilvegostomig is a PD-1/TIGIT targeting bispecific antibody that AstraZeneca acquired from Compugen, a company specializing in developing bispecific antibodies. The drug targets PD-1 and TIGIT, which are receptors that inhibit anti-cancer T-cell activities. The Phase 3 trial is being conducted worldwide, enrolling 858 patients. In South Korea, the MFDS approval grants the study to enroll 50 patients at Seoul National University, Severance Hospital, Seoul Asan Medical Center, Samsung Medical Center, Seoul St. Mary's Hospital, Seoul National University Bundang Hospital, and Seoul Boramae Hospital. The current clinical trial is a follow-up study of 'ARTEMIDE-Lung01' and 'ARTEMIDE-Lung02' to evaluate the safety of Rilvegostomig. Keytruda will be used as a control drug to Rilvegostomig, and platinum-based chemotherapy (carboplatin, paclitaxel, and lead-paclitaxel) will be used in combination. Participants will use Rilvegostomig 750 mg or Keytruda 200 mg in combination with the participant's choice of a platinum doublet chemotherapy for the first 4th cycle, administering a single dose infusion every 3 weeks. When the patients do not show clinically significant infusion response within 21 days after the second blinded trial treatment, the investigator will choose to immediately administer pemetrexed upon the completion of the blinded trial treatment, followed by administration of cisplatin and carboplatin in all other cycles. AstraZeneca has been conducting the global Phase 3 trial of Rilvegostomig in South Korea for bile duct cancer and NSCLC. Meanwhile, the data from Rilvegostomig's Phase 1/2 ARTEMIDE-01 study (NCT04995523), presented at the 2024 IASLC International Lung Cancer Summit, have shown that the drug induces continual responses and favorable drug tolerance in patients with metastatic NSCLC. When the patients were given a dose of Rilvegostomig 750 mg every 3 weeks in those with PD-L1 tumor proportion score (TPS) of 1%-49% (n=31), it resulted in an overall response (ORR) of 29%, with 38.7% continuing treatment at the time of data cutoff.
- Policy
- Cushing’s syndrome drug Isturisa is approved in Korea
- by Lee, Hye-Kyung Sep 20, 2024 05:51am
- Various doses of ‘Isturisa’ (osilodrostat), a treatment for Cushing's syndrome, are expected to be approved in Korea soon. According to industry sources on the 19th, the Ministry of Food and Drug Safety concluded the safety and efficacy review of Recordati Korea's Isturisa Film Coated Tab 1mg earlier this month and recently completed the safety and efficacy review of the 5mg dose as well. Isturisa was previously approved by the US Food and Drug Administration (FDA) on March 6, 2020, the European Medicines Agency (EMA) on January 9, 2020, and Japan’s Pharmaceuticals and Medical Devices Agency (PMDA) on March 23, 2021. Among the three dosage forms available – 1, 5, and 10 mg – the MFDS has completed a safety and efficacy review for the 1 and 5 mg doses. Isturisa has been under review for approval in Korea since November last year after being designated as a Global Innovative products on Fast Track (GIFT) by the MFDS. As the safety and efficacy review is the final step in the approval process, the drug’s approval is expected soon. Isturisa inhibits CYP1181, an enzyme responsible for the final step of the cortisol pathway in the adrenal glands, and was designated as a GIFT product in April 2022, when Novartis' ‘Signifor Inj’ was withdrawn from the market and the only existing treatment option was eliminated. The drug is indicated for the treatment of adult patients with Cushing’s disease for whom pituitary surgery is not an option or has not been curative and is taken orally twice a day. Cushing's syndrome occurs when the body is exposed to excessive amounts of a hormone called glucocorticoids. Glucocorticoids are produced by an endocrine organ called the adrenal glands, which are located on top of the kidneys and can occur when the adrenal glands produce more glucocorticoids than necessary, or when excessive amounts of glucocorticoids enter the body from the outside for various reasons. Cushing's syndrome is characterized by a rounded, moon-shaped face and excessive subcutaneous fat deposits on the back of the neck and shoulders, and is most common in adults between the ages of 30 and 50. It affects women three times more often than men. It can cause health issues such as hypertension, obesity, type 2 diabetes, blood clots in the legs and feet, fractures, a weakened immune system, and depression, and can be diagnosed through a blood test and a 24-hour urine test. Isturisa is also the first FDA-approved drug to work directly on cortisol overproduction by blocking an enzyme known as 11-beta-hydroxylase and preventing cortisol synthesis. The safety and effectiveness of Isturisa were demonstrated in a clinical study involving 137 adult patients, where approximately half of the patients reached cortisol levels within normal limits at Week 24. After Week 24, 71 patients who did not require further dose escalation and tolerated the drug participated in an 8-week double-blind, randomized withdrawal study in which withdrawals were treated with either Isturisa or placebo. Results showed that 86% of the patients in the Isturisa arm maintained cortisol levels within normal limits. On the other hand, only 30% of the placebo arm reached the same result.
- Policy
- MFDS approves Hemgenix for Hemophilia B in Korea
- by Lee, Hye-Kyung Sep 19, 2024 05:48am
- The Ministry of Food and Drug Safety (MFDS) announced on the 13th that it has approved the orphan drug ‘Hemgenix Inj (etranacogene dezaparvovec)’ imported by CSL Behring Korea. Hemgenix is used to treat moderate-to-severe hemophilia B (congenital blood clotting factor IX deficiency) in adults without a history of Factor IX inhibitors. The drug is expected to provide new treatment opportunities for hemophilia B patients by offering a long-term, single-shot treatment option, unlike existing treatments. The MFDS explained that the quality, safety and effectiveness, manufacturing and quality control standards of Hemgenixwere thoroughly reviewed and evaluated scientifically in accordance with the review criteria outlined in the “Act on The Safety of and Support for Advanced Regenerative Medicine and Advanced Biological Products (“Advanced Regenerative Bio Act”),” which enabled the product’s expedited review and prompt introduction into the field. Hemgenix will be subject to long-term follow-up under Article 30 of the Advanced Regenerative Bio Act, which requires pharmaceutical companies to follow up on the occurrence of adverse events for 15 years from the date of administration. The MFDS said, "Based on our expertise in regulatory science, we will continue to make our best efforts to ensure that novel therapies for severe and rare diseases are promptly supplied to patients in Korea.”
- Policy
- Moderna’s COVID-19 vaccine is approved in Korea
- by Lee, Hye-Kyung Sep 13, 2024 05:50am
- A new COVID-19 variant vaccine, which is the only mRNA-based COVID-19 vaccine that will be manufactured domestically (by Samsung Biologics) has been approved in Korea. The Ministry of Food and Drug Safety (MFDS, Minister: Yu-Kyoung Oh) announced on the 11th that it has authorized the manufacturing and sale of ‘Spikevax JN.1’ that Moderna Korea applied for. Like Pfizer's COVID-19 vaccine, which was approved on August 30, Spikevax JN.1 is a vaccine that contains an mRNA designed to express the JN.1 variant antigen as the active ingredient. It is indicated for the prevention of COVID-19 in persons 12 years of age and older and is administered as a single intramuscular injection of 0.5mL. Those who have previously received a COVID-19 vaccine should administer Spikevax JN.1 at least 3 months after his or her most recent COVID-19 vaccination. Samsung Biologics will receive the active pharmaceutical ingredient supplied by Moderna and manufacture the finished drug through filling and labeling, and its domestic manufacture is expected to ensure a smooth supply of the vaccine. The Ministry of Food and Drug Safety said, ‘While strictly examining the safety, effectiveness, and quality of this vaccine, we worked to promptly approve the drug in 2 months so that there would be no disruption to the National Immunization Program for high-risk groups that are scheduled to begin next month.”
- Policy
- Price of Pristiq original and IMDs cut with generic release
- by Lee, Tak-Sun Sep 11, 2024 05:54am
- PfizerThe release of generic versions of Pfizer's antidepressant ‘Pristiq ER Tab,’ has hit not only the sales of the original drug but also the salt-modified version. Korea Pharma launched the first generic version of Pristiq in Korea last month, and the release has also affected the salt-modified drug that was released 4 years ago. According to industry sources on the 9th, the upper insurance price limit of the original Pristiq ER Tab and the salt-modified drug received ex officio adjustments upon the entry of the generic version. The insurance price of the items will remain at 70% of the maximum price for 1 year but then be reduced to 53.55% like the generic’s price. Desvenlafaxine is a serotonin-norepinephrine reuptake inhibitor (SNRI), which is characterized by its low risk of drug interactions and a low risk of side effects such as hypertension and sexual dysfunction. Due to such advantages, the drug has become a popular choice in the antidepressant market. According to IQVIA sales, the original Pristiq generated sales of KRW 7.2 billion last year. With the listing of the generic drug, its upper insurance price limit will be reduced to 70% from September. As a result, the price of Pristiq 50mg ER Tab will be reduced from KRW 1,002 to KRW 702, and Pristiq 100mg ER Tab will be adjusted to KRW 873. This was an ex officio adjustment of the upper limit upon the reimbursement listing of Korea Pharma’s generic drug. The upper limit of the original drug is adjusted to 53.55% of the initial price when a product with the same route of administration, ingredients, and dosage form is introduced for the first time, but then is set at 70% of the original price for one year. In addition to the ‘Pharma Desvenlafaxine ER Tab 100mg’ that Korea Pharma received reimbursement listing last month, the company has listed ‘Pharma Desvenlafaxine ER Tab 50mg’ with reimbursement this month. Both are generic drugs that contain the same active ingredient (desvenlafaxine succinate monohydrate) as Pristiq. The generic listing also affected the price of salt-modified versions of the drug that were released 4 years ago. The price of Whan In Pharm (desvenlafaxine), Myeongin Pharm, Hallim Pharmaceutical, and Nexpharm Korea (desvenlafaxine benzoate) was also reduced to 70% of the initial price. This is because when the price of the development target product (original Pristiq ER Tab) is adjusted, the price of the salt-modified drugs is also reduced together. No price adjustments had been made until now as only salt-modified versions with different ingredient names were listed, with no generic versions. The price of the salt-modified versions was set at 90% of the target product's price upon initial listing. However, generic products were introduced 4 years after the launch of the salt-modified drugs, rendering price adjustments of all the previously introduced drugs inevitable. The salt-modified drugs were developed to avoid patent infringement and introduced to the market in 2020. The patent for the original Pristiq ER Tab expired in October 2022. The price of the original and the salt-modified versions will be reduced to 53.55% after 1 year. An industry official said, “With the launch of the generic, the 4-year coexistence between the original and the salt-modified drug has come to an end. Due to the price cut, sales of the existing drugs will inevitably decline.”
- Policy
- MFDS announces EUA application of new COVID-19 vaccine
- by Lee, Hye-Kyung Sep 09, 2024 05:49am
- An emergency use authorization process is in progress for new COVID-19 vaccines so that the disease control authorities can inoculate using the vaccines in October. On the 6th, the Ministry of Food and Drug Safety announced an application for emergency use approval of the ‘JN.1 variant-response recombinant protein vaccine for the prevention of COVID-19 caused by SARS-CoV-2 virus’. The EUA system allows vaccines requested by the Commissioner of the Korea Disease Control and Prevention Agency to be manufactured and sold for a limited time if there is no approved product in Korea. With the frequent reemergence of infectious diseases that threaten mankind, such as the swine flu and COVID-19, the U.S. Food and Drug Administration (FDA) established the Emergency Use Authorization (EUA) system to exempt the authorization process of medical devices that are in urgent need due to infectious disease pandemics. In Korea, the EUA was first introduced in 2016 for MERS, and during the COVID-19 outbreak, many vaccines and treatments were actively approved using the EUA system. The EUA application notification this time is for 320,000 doses of a new COVID-19 vaccine, which is believed to be Novavax's JN.1 COVID-19 vaccine, which the KDCA signed an agreement for in July. The KCDA said it has secured 5.23 million doses of Pfizer’s vaccine, 2 million doses of Moderna, and 320,000 doses of Novavax’s vaccine, as new COVID-19 vaccines to be used in the 2024-2025 season starting in October. Two of the vaccines that the KDCA procured the most – Pfizer's Comirnaty JN.1 COVID-19 Inj (bretovameran) (Sars-coronavirus-2 mRNA vaccine) and Comirnaty JN.1 Inj (single-dose vial) - have already been granted marketing authorization in Korea. Pfizer had first applied for marketing authorization of ‘Comirnaty Bivalent Inj,’ which is used for the existing pandemic variant, to expedite the approval of the new vaccine, by leaving a GMP review history in place. To receive formal approval for their COVID-19 vaccines, the companies need to submit data on non-clinical trials, clinical trials, quality and risk management plans, and manufacturing and quality control for marketing authorization and review. On the other hand, for EUA, the following requirements need to be satisfied: ▲ the applicant needs to be a drug manufacturer or importer; ▲ demonstrate that the drug is effective against the JN.1 variant of COVID-19 caused by the SARS-CoV2 virus; ▲ demonstrate that the safety and quality of the drug is ensured; ▲ and, in the case of imported products, the products need to have received measures equivalent to approval in a foreign country that conducts drug safety control at a level equal to or higher than that of Korea. During the last COVID-19 outbreak, the EUA system was used to shorten the document preparation period from 30 days to 7 days, the protocol approval and clinical trial period from 90 days to 22 days, and the final review and approval period from 80 days to 30 days.
- Policy
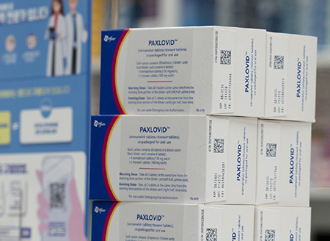
- COVID-19 drug Paxlovid’s price likely to be based on Japan
- by Lee, Tak-Sun Sep 06, 2024 05:48am
- The insurance ceiling price of Pfizer's COVID-19 drug Paxlovid is likely to be set at around KRW 900,000 in Korea. This is similar to its price in Japan. Japan is said to have the lowest price for Paxlovid among the A8 countries. According to industry sources on the 4th, Paxlovid passed the Drug Reimbursement Evaluation Committee (DREC) on the 29th of last month after undergoing economic evaluation. The drug will be registered for health insurance reimbursement benefits after the company negotiates the drug price with the National Health Insurance Service. The key is its price. DREC reportedly deliberated on a price in the KRW 1 million range and approved the drug’s reimbursement as adequate. However, the NHIS is expected to focus on lowering the price further through negotiations, and the final price is likely to be around KRW 900,000. In Japan, which has the lowest price among the A8 countries, 1 set (5-day supply) of Paxlovid is reportedly priced at JPY 99,027. At the current exchange rate, that's about KRW 920,000. It is analyzed that the price, which was initially in the KRW 1 million range, has dropped to KRW 920,000 upon Japan’s yen falling. The NHIS is also expected to negotiate Korea’s drug prices based on Japan’s prices. However, timing is of issue. The NHIS only has about 20 days to negotiate to meet the October deadline set by the Ministry of Health and Welfare. Add to that the Chuseok holiday and the NHIS negotiation team will be under much pressure to lower the price and complete the registration process quickly. Currently, the government purchases the drug, and patients pay KRW 50,000 for the drug. If it is listed for reimbursement at KRW 1 million, at the current co-payment rate of 30%, patients will have to pay KRW 300,000. If this happens, the patients’ out-of-pocket expenses will skyrocket, which will cause a public backlash. This is why the government is pushing to lower the co-insurance rate. On the 3rd, the Ministry of Health and Welfare announced a proposed amendment to the Enforcement Decree of the National Health Insurance Act to reduce the co-insurance rate for patients with infectious diseases. Accordingly, the drug pricing negotiations and the adjustment of the co-insurance rate for Paxlovid will be conducted simultaneously this month. This will determine the final price paid by the patients. “Looking back at the past drug pricing negotiations, I think the price of Paxlovid will be adjusted to a level lower than the price accepted by DREC during the HIRA negotiations,” said a pharmaceutical industry insider, “but unlike the government, Pfizer is not in a hurry, so the NHIS will have a lot to worry about.”