- LOGIN
- MemberShip
- 2025-12-21 09:34:07
- Policy
- 5-year relative survival rate of cancer 72.1% in 2021
- by Lee, Jeong-Hwan Jan 02, 2024 05:45am
- The five-year relative survival rate for cancer patients increased by 6.6% points in 10 years and has become 72.1%. In Korea, thyroid cancer was the most common, followed by colorectal, lung, and stomach cancers. On December 28th, the Ministry of Health and Welfare (Minister Kyoo-Hong Cho) and the Central Cancer Registry Cancer (National Cancer Center, Director Hong-Gwan Seo) released the 2021 National Cancer Registry statistics (cancer incidence, relative survival rate, prevalence, etc.). The number of new cancer cases in 2021 was 277,523, an increase of 27,002 (10.8%) compared to 2020. This is analyzed to be a result of a resurgence in the use of healthcare services, including cancer screenings, which had decreased due to the COVID-19 pandemic, and an expansion of the scope of registration screening subjects made according to changes in cancer registration guidelines. The most common cancer in 2021 was thyroid cancer (35,303, up 19.1% from 2020), followed by colorectal, lung, stomach, breast, prostate, and liver cancers. The incidence of stomach, colorectal, liver, and cervical cancers, which are cancer types targeted by the National Cancer Screening Program, has been decreasing for the past decade, while the incidence of breast cancer has been increasing for the past 20 years. The 5-year relative survival rate for cancer patients diagnosed in the last 5 years ('17-'21) was 72.1%, indicating that 7 out of 10 cancer patients survived for more than 5 years. The 5-year relative survival rate for cancer patients has continued to increase and is 6.6% points higher than the rate found for cancer patients who were diagnosed around 10 years ago (’06-’10, 65.5%). As of January 1, 2022, 2,434,089 people had cancer. 1 out of every 21 people (4.7% of the total population) had cancer, and 1 out of every 7 people aged 65 and older (1,194,156 cancer patients) had cancer. In particular, as of 2021, more than half (60.8%) of people with cancer survived for more than 5 years after being diagnosed, amounting to 1,795,366, which is an increase of 111,396 survivors compared to the previous year (1,361,840 survivors).
- Policy
- Revising the PE exemption system… focuses on 'deferral'
- by Lee, Tak-Sun Jan 02, 2024 05:44am
- The ‘Pharmacoeconomic Evaluation Exemption System', which was first implemented in 2015, will be completely transformed in the new year. In the future, the system will defer rather than exempt companies from submitting required data, increasing the possibility of drugs being evaluated after listing. According to the industry on December 29th, the study on 'Preparation of a plan to improve the pharmacoeconomic evaluation data submission waiver system’ that was conducted as the Health Insurance Review and Assessment Service’s research service in February, has been completed. The results of the study, which mention the need to redesign the system to defer data submission rather than omit it, are expected to be used to make systemic improvements. As a result, drugs subject to deferral of pharmacoeconomic evaluation data submission will also prepare evidence for the agreements it had made when it was listed through prior assessments. The system, which was implemented in 2015, is applied to rare disease drugs and anticancer drugs for which no alternatives exist. This year, it was also applied to pediatric drugs that have proven to improve quality of life. However, the HIRA believes that these drugs need to undergo a post-marketing cost-effectiveness evaluation, given how expensive these drugs are. The need for post-marketing evaluation of PE exemption drugs was also mentioned at the public hearing for the ‘Performance-based reimbursement management plan for drugs using RWD/RWE’ that was held last November. At the time, Mi-Young Yoo, Director-General of the Pharmaceutical Benefits at HIRA, said, “Since the introduction of the positive listing system in 2006, many drugs have been listed for reimbursement through various systems including the PE exemption system to enable better patient access. So this is now the time a post-listing measure needs to be implemented. Although social consensus should be made on its need, such a management system can be a way to ensure an appropriate level of financial soundness within limited insurance.” This implied that RWD (Real-World Data) can be used to post-evaluate drugs that have omitted pharmacoeconomic evaluations. At the ‘2023 Korean Association of Health Technology Assessment Winter Conference' that was held on the 1st of the previous month, experts raised voices that the system should be redesigned so that the exemptions are switched to deferrals. Accordingly, HIRA is expected to improve the overall system to introduce post-evaluation of PE exemption drugs this year, based on the results of the research service.
- Policy
- Peramiflu shortages may require gov. intervention
- by Lee, Tak-Sun Dec 29, 2023 05:39am
- The government is poised to implement supply control of Peramiflu inj., an injection for transfusion, following the management of oral influenza treatment, Tamiflu. Peramiflu inj. is experiencing out-of-stock in medical services due to a recent increase in demand. Health Insurance Review and Assessment Service (HIRA)’s Korea Pharmaceutical Information Service (KPIS) designated two types of Green Cross’s Peramiflu Inj. (peramivir), after receiving reports through the information channel, as drug shortages, and plans to provide inventory information on these drugs. The information service has been operating a channel for receiving reports on drug shortages since July. Reporting on drug supply shortages is open to anyone, including associations, groups, doctors and pharmacist, and the public. HIRA discloses information on the inventory of drugs that are experiencing supply shortages by analyzing distribution status and identifying drugs currently facing supply issues. Until now, Peramiflu Inj. has not been registered on the drug shortages list. However, remaining stocks of three oseltamivir products, including Tamiflu, have been distributed following the drug shortages designation. Regarding Tamiflu, the government released Tamiflu from the national drug reserve into the market. Starting last week, pharmacists have been gradually releasing the stock for 180,000 people. Green Cross’s Peramiflu is an original drug that contains peramivir as active ingredient. Although it is a non-reimbursed drug, there are 15 generics available in the market. Generic drugs have not been reported to the drug shortages information channel. “HIRA is currently assessing management strategy to address the drug shortages; for example, sharing information about the drugs that have been reported through the information channel with a public-private consultative body,” stated a representative from the HIRA. The issue of Peramiflu abuse was discussed during the second meeting of the 'respiratory diseases joint-departments taskforce' on the 27th. Medical experts, including those from Korean Society of Pediatric Infectious Diseases and The Korean Pediatric Society, have expressed concerns that healthcare providers prioritize the prescription of injections over oral pills, despite both being equally effective. Peramivir ingredient is designated as a national essential medicine. Therefore, whether the government will actively pursue drug supply management for peramivir ingredient is of interest.
- Policy
- True Set, a triple hypertension therapy, to face generics
- by Lee, Tak-Sun Dec 28, 2023 06:02am
- Generics of Yuhan’s True Set Tab., a triple-combination drug for hypertension with rapid sales growth, are already gearing up for competition. True Set, a triple-combination drug that contains telmisartan, amlodipine besylate, and chlorthalidone, received approval in August 2019. Subsequently, True Set was released to the market in November following reimbursement approval. True Set’s re-examination period is set to expire in August 22, 2025, which is a year and 8 months from now. Given these circumstances, generic companies are actively pursuing opportunities for generic entry. The MFDS approved Jeil Pharm’s bioequivalence trial protocol for JLP-2202 on 21st. A comparative drug contains Telmisartan 80mg, Amlodipine Besylate 6.935mg, and Chlorthalidone 25mg as active ingredients. A currently authorized drug for the market is True Set Tab. 80/5/25mg. Released in November 2019, True Set Tab. recorded an annual outpatient prescription sales of 10 billion won, in just two years. According to the data from UBIST, True Set Tab.’s outpatient prescription sales recorded 16.8 billion won, with a cumulative outpatient prescription sales in Q3 reaching 13.4 billion won, breaking last year’s record and showing potential for rapid growth. Currently, Daiichi Sankyo Korea’s Sevikar HCT (Olmesartan Medoxomil/Amlodipine Besylate/Hydrochlorothiazide), Amosartan Plus (Amlodipine Camsylate/Losartan potassium/Amlodipine Camsylate), and True Set (Telmisartan/Amlodipine Besylate/Chlorthalidone) are dominating the triple-combination drug market. Among these, generics for Sevikar HCT has already been released in the market. Amosartan Plus and True Set remain exclusive in the market. However, drug product patent for Amosartan Plus is expiring in November 2036. Additionally, Amosartan Plus contains Amlodipine Camsylate, which is exclusively produced by Hanmi Pharm, making it difficult for generic companies to approach immediately. Since True Set does not have a relevant patent, and its re-examination is set to be completed three years from now, generic companies have been eyeing the drug. Korean pharmaceutical companies are facing limited opportunities for generic development due to the scarcity of original drugs with expiring patents. Therefore, many companies, including Jeil Pharm, are awaiting to seize the opportunity to manufacture True Set generics.
- Policy
- Reform should drive development of 2 homegrown blockbusters
- by Lee, Jeong-Hwan Dec 27, 2023 06:03am
- The government expressed the will to encourage pharmaceutical companies to invest in research and development (R&D) and secure the momentum of developing two homegrown blockbuster drugs through the reform of the drug pricing system to reflect innovative value. Above all, the government has made it clear that it will strengthen the sustainability of national health insurance finances by reducing the proportion of pharmaceutical expenses, and at the same time, investing the funds generated by trimming the insurance drug prices of drugs that violate the purpose of selective benefits into innovative new drugs and essential drugs. In particular, the government said it had devised the reform of the drug pricing system to strengthen the supply chain of essential drugs in terms of health security, which arose as a key issue of concern during the COVID-19 pandemic. On the 22nd, Director Chang-Hyun Oh, Director of Pharmaceutical Benefits at MOHW, said at a meeting with the press corp to explain the implications of the 'Plan to Reflect the Innovation Value of New Drugs and Improve the Drug Price System for Health Security' that was recently passed by the Health Insurance Policy Review Committee. The Ministry of Health and Welfare will revise the drug pricing system to favor the drug prices of domestically developed new drugs made by innovative pharmaceutical companies and support the export of domestic new drugs at the listed price after applying the risk-sharing agreement system homegrown new drugs exported overseas. The government will also ease regulations on drug price reductions based on the Price-Volume Agreement system and establish regulations on preferential drug prices for botanical drugs. New drugs that are recognized as innovative will be exceptionally recognized for cost-effectiveness even if they exceed the ICER threshold during pharmacoeconomic evaluations and will be applied eased evaluation standards when being reviewed for RSS renewals. Also, the government will provide preferential pricing for drugs based on natural products that demonstrate superiority and innovation. To strengthen the national security of pharmaceuticals, a system will be operated to grant a 68% drug pricing premium for up to 10 years (basic 5 years, additional 5 years) for national essential drugs that use domestic APIs. Chang-Hyun Oh, Director of Pharmaceutical Benefits at MOHW explains the background and goals of the reform of the drug pricing system reflecting innovation value In addition, the evaluation criteria for adjusting the upper limit for national essential drugs will be relaxed, and the cost preservation procedure will be simplified, through measures such as ordering prior drug pricing negotiation, if the cost increase factor of supply and demand insecurity drugs is proven. Oh said he hopes the reforms will lead to stronger investment in new drug R&D by pharmaceutical companies and the development of real blockbuster drugs. "Until now, we have streamlined many procedures to strengthen coverage of serious drugs. However, there were not many cases where we raised the appraisal value of drugs (preferential drug prices).” So this time, we seek to first focus on rewarding innovative value (during drug pricing). This will encourage pharmaceutical companies to invest more in R&D, which will increase jobs and lead to the development of new drugs." Oh continued, "Korea is aiming to develop two blockbuster drugs by 2027, and for that, there needs to be a drive that recognizes innovative value within the national health insurance system. Next, the global supply chain has been severely disrupted by COVID-19. We did a lot of work last year, such as urgently raising the price of acetaminophen, but in the end, we concluded that it is important to increase localization and self-sufficiency of necessary drugs." "We devised a reform plan that emphasizes the need to create an environment for domestic pharmaceutical companies to produce their own drugs, with the belief that this, to a certain extent, would stabilize drug supply during disasters such as the spread of infectious diseases. Adding premium pricing for drugs using APIs from Korea and limiting it to national essential drugs was to build external rationale, as well as conflict with the FTA and WTO trade issues. Also, we were worried that creating a system that favors only our country would violate the law, and prioritize national essential drugs because of their rightful preferential status." Regarding the revision of the Price-Volume Agreement system (PVA), Oh said that a proposal to adjust the price discount imposed on drugs by a certain percentage is likely for drugs that are subject to price reductions more than 3 times in 5 years. However, he said that it is difficult to disclose the exact percentage. For example, when the domestic new drug K-CAB was repeatedly subjected to PVA price cuts, the ministry said that if the developer, HK Inno. N, was designated as an innovative pharmaceutical company, part of the price reduction would be removed. When asked how the government plans to balance drug costs in health insurance finances, Oh said, "Currently, drug costs account for 23.3% of NHI medical expenditures, and I don't know how much it will go down (with the reform), but we are aiming for 21% to 22%. We will continue to narrow down drugs that do not meet the purpose of selective reimbursement. Also, we're going to cut reimbursement of drugs that don't fit the actuarial principle of the system. Naturally, there will be savings, and if we use them for innovation, it may serve as an incentive for pharmaceutical companies to develop new drugs."
- Policy
- Swiss’s Idorsia applies for the reimb of its first product
- by Lee, Tak-Sun Dec 27, 2023 06:03am
- The Korean subsidiary of the Swiss pharmaceutical company Idorsia has started the reimbursement process for the drug upon receiving approval for Pivlaz Inj (clazosentan sodium). The drug, which is used to prevent cerebral vasospasm, is expected to be sold by Handok in Korea, with the company also conducting domestic clinical trials. According to industry sources on the 26th, Idorsia Pharmaceuticals Korea (President: Minbok Lee) recently applied for the reimbursement of its Pivlaz Inj to the Health Insurance Review and Assessment Service. The company quickly started the reimbursement listing process after obtaining marketing authorization from the Ministry of Food and Drug Safety on July 7. The drug is a selective endothelin A receptor antagonist indicated for the prevention of cerebral vasospasm, vasospasm-related cerebral infarction, and cerebral ischemic events in adults who have undergone craniotomy or procedures after aneurysmal subarachnoid hemorrhage. The company explained that Pivlaz is the first drug approved in Korea to prevent both cerebral vasospasm and its complications. At least 25% of patients diagnosed with aneurysmal subarachnoid hemorrhage die, and approximately 50% of survivors suffer neurological deficits. Globally, the disease affects 6.7 people per 100,000 people per year and 9 people per 100,000 in Korea. In a Phase III trial that was conducted in Japan, Pivlaz significantly reduced the incidence of cerebral vasospasm-related complications and all-cause mortality within 6 weeks of subarachnoid hemorrhage, which confirmed its safety. Another Phase II trial that was jointly conducted in Korea and Japan enrolled 74 Korean patients. Handok has been conducting domestic clinical trials and licensing the product in collaboration with Idorsia. Both are expected to jointly take charge of reimbursement and sales as well. Idorsia recently launched its insomnia drug Quviviq in the U.S. and Europe, and arose as one of the hottest pharmaceutical companies in the country, recording sales of KRW 100 billion in Q2 2022 alone. Domestic clinical trials for Quviviq have also been carried out by Handok since 2019 in Korea. Japan’s Sosei Group holds all of the sales rights for Quviviq. In July, the Sosei Group acquired Idorsia's pharmaceutical business in the Asia-Pacific region, excluding China, for approximately 65 billion yen. With the acquisition, Sosei Group now reportedly holds all of the shares of Idorsia's Japanese and Korean subsidiaries. In addition to Pivlaz, Sosei plans to market insomnia treatment Quviviq and up to seven other products from Idorsia's global pipeline in Asia-Pacific.
- Policy
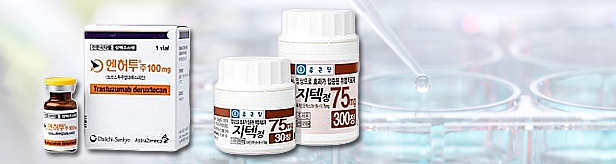
- Enhertu, G-tec will benefit from new govn't plan
- by Lee, Tak-Sun Dec 26, 2023 05:47am
- According to the ‘Plan for the compensation of the innovative value of new drugs’ that the government announced on the 22nd, the breast cancer treatment ‘Enhertu (Daiichi Sankyo-AstraZeneca),’ and the new gastrointestinal botanical drug ‘G-tec (Chong Kund Dang)’ are being regarded as immediate beneficiaries. In the case of Enhertu, it is expected to receive a reimbursement and make way for its reimbursement according to the benefit plan for innovative new drugs according to preferential price awarded to new innovative drugs.' G-tec will receive preferential treatment as a new botanical drug. The burden of drug price cuts for new products produced by innovative pharmaceutical companies will also be reduced based on the eased Price-Volume Agreement system. The government decided to accept reimbursement of innovative new drugs that are recognized by the state. as an innovative new drug, even if they exceed the drug’s ICER threshold, an economic evaluation indicator. The new breast cancer drug Entertu is being evaluated as the only new drug that satisfies the government’s innovativeness standards. The criteria for innovativeness are ▲ there is no substitute or therapeutically equivalent product or treatment ▲ demonstrated clinically meaningful improvement, such as a significant extension in survival ▲ the new drug has been approved by the Ministry of Food and Drug Safety under Article 35(4)(2) of the Pharmaceutical Affairs Act (designation of priority review) and were approved through the fast-track (GIFT) or received a breakthrough therapy designation (BTD) by the US FDA or a priority review (PRIME) by the European Union’s EMA. Enhertu met all of these criteria and is expected be applied a flexible ICER threshold. Enhertu’s reimbursement process is stuck at the pharmacoeconomic evaluation stage because it improved life expectancy and rather increased treatment cost per patient. For example, if the ICER threshold exceeds KRW 50 million, its cost-effectiveness is not recognized, making it difficult to pass the pharmacoeconomic evaluation. However, in this improvement plan, a measure to accept drugs whose innovativeness is recognized, therefore, the drug’s reimbursement progress gains momentum. In addition, Chong Kun Dang’s new drug G-tec will likely benefit and be eligible for preferential drug pricing as a new botanical drug during the reimbursement process. G-tec is a cinnamon bark dried extract that was granted marketing authorization in July last year. The improvement plan reportedly includes preferential drug pricing for drugs developed by innovative pharmaceutical companies. for non-inferior new botanical drugs and new botanical drugs. As a result, there is a possibility that drug prices that were previously set below the weighted average price of alternative drugs or be set in between the highest weighted average price and the weighted average price of alternative drugs. This means that drug prices will be set slightly higher. Chong Kun Dang is an innovative pharmaceutical company, and G-tec is a new botanical drug, so it is likely that the two drugs will both benefit through reimbursement negotiations. On the other hand, Jeil Pharmaceutical’s new Gastroesophageal Reflux Disease (GERD) drug ‘zastaprazan,’ which is considered a potential novel homegrown drug candidate for commercialization next year, is not eligible for this improvement plan. This is because neither Jeil Pharmaceutical nor the drug’s developer, Onconic Therapeutics, is regarded as an innovative pharmaceutical company. Although not immediately eligible, new products from innovative pharmaceutical companies will be able to ease the burden of drug price cuts as they are applied to an eased PVA system. The improvement contains a plan that lowers the drug price cut rate for drugs produced by innovative pharmaceutical companies or an equivalent if the drug is subject to continued PVA price cuts - three times in five years, due to a continuous increase in usage. As a result, products that were subject to more than 3 out of 5 PVA price cuts will receive a reduced price cut rate next year. However, the key is the timing of implementation. The government plans to apply the measures sequentially from the beginning of next year, and the outline of eligible products is expected to be clarified depending on the timing of the revision. An official from the domestic pharmaceutical industry said, "The proposed new drug value compensation plan will at least induce the development of domestically developed drugs, increasing their motivation to develop new drugs.” "This is why domestic pharmaceutical companies have long desired preferential drug pricing for innovative pharmaceutical companies," he said.
- Policy
- Series of expectorant Prospan generics enter KOR mkt
- by Lee, Tak-Sun Dec 22, 2023 05:46am
- Generic versions of Prospan Syrup, a drug that dominated the phyto-expectorant market in the 2000s, are again being introduced to the market. Prospan Syrup, which has been resold by Kwangdong Pharmaceutical since 2012, is the only available 200mL bottle formulation of Prospan, and 7.5mL and bottle formulations of the drug are only available from Kwangdong Pharmaceutical and Youngjin Pharmaceutical. However, 500mL bottle formulations from Ildong Pharmaceutical, Sama Pharm, and Pharmgen Scien are available with reimbursement. In total, 5 companies are selling ivy leaf dried extracts (dried extract of ivy leaves (extraction solvent, 30% ethanol), the active pharmaceutical ingredient in Prospan Syrup. In this situation, four companies will be listed for reimbursement at once next month. According to the industry on the 21st, Ilsung Pharmaceuticals, Kuhnil Biopharm, and Daewoong Bio's Ivy Leaf 30% Ethanol Dried Ext 7.5mL package products will be listed on the reimbursement list from the 1st of next month. Also, Nexpharm Korea and Ilsung Pharmaceuticals’ 500mL vial product will be applied reimbursement. As there are more than 2 but less than 19 identical preparations available in the market, Prospa Syrup generic companies can receive the highest price if they meet the pricing criteria. The products on the list met all the requirements and received the highest price of KRW 240 per packet and 32 won per mL bottle. Prospan syrup was the leading phyto-expectorant with a market share of 25% in the 2000s. In 2010, UBIST statistics show that outpatient prescription sales for the drug alone reached KRW 37.8 billion. The frog character on the product package reflected the popularity of Prospan alone. The drug, which was introduced by Ahn-gook Pharm in 2010 from Germany's Engelhard, suffered a downturn due to its switch to an over-the-counter drug. In 2011, the drug was reevaluated by the Ministry of Food and Drug Safety (MFDS) and converted to an over-the-counter drug, and in that year, the was covered by health insurance only for people under 12 years of age based on the principles set for the oral liquid formulation. Ahn-gook Pharm released Synatura, a combination drug that contains Prospan in March 2011, and parted ways with Prospan in September of the same year. After seemingly ending its relationship with the domestic market, Prospan was reintroduced to the Korean market by Kwangdong Pharmaceutical in 2012 and has remained available ever since. However, Prospan failed to regain its former glory due to the rise of the use of combination drugs such as Synechura. According to IQVIA statistics, Prospan’s sales last year were only KRW 500 million. Nevertheless, there are reasons why generic companies are launching their respective versions. First of all, the number of generics is small, so there are no concerns about receiving discounted prices through the stepped pricing system. Moreover, over-the-counter syrups do not have to meet the ‘own bioequivalence testing’ requirements, so there is no burden on contract manufacturers. All of the pharmaceutical companies that have received the salary this time are being supplied the drug in consignment from Daewon Pharmaceutical. Another favorable factor is that adults can be prescribed Prospan with reimbursement following the change in reimbursement standards that were made in February 2019. In addition, Kwangdong Pharmaceutical's launch of a conveniently packaged product in 2021 has also contributed to the upward trend. Above all, the rise in demand for respiratory drugs after COVID-19 is likely to have attracted the entry of new generics. More Prospan syrup generics are expected to be introduced to the market. Three more pharmaceutical companies received approval for the product, including Daewon Pharmaceutical, Ilhwa, and Hutecs Korea Pharmaceutical.
- Policy
- Delayed re-evaluation of hyaluronic acid eye drops
- by Lee, Tak-Sun Dec 21, 2023 05:54am
- The re-evaluation of the reimbursement appropriateness of hyaluronic acid (HA) eye drops has ultimately been delayed. On the 7th, the Health Insurance Review and Assessment Service (HIRA)’s Drug Reimbursement Committee decided to conduct an additional review of the re-evaluation item. Similarly, on the 20th, the Ministry of Health and Welfare (MOHW)’s Health Insurance Policy Review Committee was unable to reach a decision. Experts who reviewed the re-evaluation item expressed concerns about the potential impact of limiting the amount of HA eye drops use on other single-use eye drops. As the re-evaluation process goes back to the beginning, it will take some time for the results to be determined. On the 20th, the Drug Reimbursement Committee stated during a meeting that, "Regarding HA eye drops, the evaluation results have indicated that establishing a comprehensive reimbursement criteria on single-use eye drops may be necessary, considering the transition to alternative single use eye drops. We will soon make a final decision on this matter." Initially, based on the initial evaluation report by the Drug Reimbursement Committee in September, HA eye drops were deemed unsuitable for reimbursement for conditions related to exogenous factors, such as post-surgery use, medication-related issues, trauma, and contact lens wear. On the other hand, endogenous conditions like Sjogren's syndrome, Stevens-Johnson syndrome, and dry eye syndrome were found to be appropriate for reimbursement. Yet, it was deemed necessary to establish reimbursement criteria, including restrictions such as limiting prescriptions to one per patient visit and setting an annual prescription limit per patient, to ensure appropriate usage. Considering that endogenous diseases make up more than 80% of all prescriptions, pharmaceutical companies were somewhat relieved by the outcomes of the initial review. In fact, no objections were raised by pharmaceutical companies in response to the initial results. However, there is concern about limiting the volume of use. Pharmaceutical companies have expressed concern about discussions to limit the amount of annual use to four from the current 60 annual uses, as it would reduce the track record by half. Despite these concerns, it is reported that no objections were filed as the re-evaluation results were not too bad. Additionally, revising the reimbursement criteria to limit the amount of use may not be straightforward due to opposing opinions among experts. In fact, some experts have suggested that the review of limiting the amount of use should be withdrawn. With the October parliamentary audit season season, there was a surge of concerns about weakened access for senior patients and potential for higher costs, creating an unfriendly atmosphere towards the HIRA. Despite HIRA's efforts to dispute media reports suggesting a more than tenfold increase in the cost of non-reimbursed drugs, there was an ongoing anxiety among the public. During the parliamentary audit season, there was a strong call from members of opposition party to maintain the reimbursement for HA, and the HIRA seemed preoccupied with appeasing the members. Amidst these developments, there were rumors circulating before the final decision in December that reimbursement might be retained for post-LASIK surgery and other exogenous conditions. This proposal would represent a reversal from the initial review. In these circumstances, it’s reported that consultations with experts regarding limiting the amount of usage have not advanced. Experts voiced concerns about a potential balloon effect after the Drug Evaluation Committee's final evaluation. They anticipated that limiting the amount of use of HA eye drops might increase volume of usage of other single-use eye drops. As a result, there is a prevailing opinion that a review of reimbursement criteria for all single-use eye drops should be conducted. However, it is perceived that if the committee were to review the reimbursement criteria for all single-use eye drops, including HA eye drops, it could be challenging to reaching a conclusion in a short time. "Revising the reimbursement criteria for all single use eye drops would pose challenges in terms of time and gathering expert opinions. Consequently, it is possible that the re-evaluation of HA eye drops may not reach a conclusion," said a representative from the pharmaceutical company. It appears that the HA eye drop companies, which had entered into preemptive contracts with prominent law firms at significant cost, have seen their desires fulfilled.
- Policy
- Braftovi Cap. & Bosulif tablets reimb for the New Year
- by Lee, Tak-Sun Dec 21, 2023 05:39am
- Starting on Jan 1 next month, two anti-cancer drugs will be reimbursed. These drugs include Ono Pharmaceutical Korea’s Braftovi Cap. 75mg (encorafenib) and the 3 Pfizer Korea’s Bosulif tablet tiems. Braftovi has been listed following drug price negotiation with the National Health Insurance Service, and Bosulif was not subject to maximum reimbursement amount negotiations. According to the industry on 19th, two anti-cancer drugs including Braftovi Cap. 75mg and Bosulif tablets in dosages of 100mg, 400mg, and 500mg will be listed for reimbursement starting on Jan 1, 2024. Braftovi tablets are used in combination with cetuximab for the treatment of adult patients who have previously received systemic therapy, with metastatic colorectal cancer (mCRC) harboring a BRAF V600E mutation. In August, both drugs successfully cleared the Health Insurance Review and Assessment Service (HIRA)’s Drug Reimbursement Evaluation Committee review, and in September, they initiated drug price negotiations with the National Health Insurance Service. The pharmaceutical companies agreed to apply the risk-sharing agreement (RSA) scheme, leading to their reimbursement approval. The drugs were applied a refund type and expenditure cap type RSA, with an agreement to submit data, such as duration of life for patients who used the drugs, at the end of the RSA period for evaluation. The maximum listed insurance price is reported to be 56,023 won per tablet. Bosulif is indicated for the second-line or later treatment of adult patients with chronic phase, accelerated phase, or blast phase Philadelphia chromosome-positive chronic myelogenous leukemia (Ph+ CML) who have previously demonstrated resistance or intolerance to neoadjuvant therapy including imatinib. In September, the drugs were cleared by the Drug Reimbursement Committee, and a decision was reached to accept an amount below the standard for negotiation exemption. As a result, negotiations on the maximum listed price with the National Health Insurance Service were bypassed, and agreement was reached only on the anticipated claim amount. The government set the maximum listed prices of Bosulif 100mg, Bosulif 400mg, and Bosulif 500mg at 23,552 won, 62,526 won, and 70,655 won, respectively, per tablet. Bosulif is a second-generation targeted anti-cancer drug available alongside Tasigna, Sprycel, and Supect. It received approval from the U.S. Food and Drug Administration in 2021 but has yet to enter the market in Korea. The competition between Pfizer and industry leaders like Novartis and Bristol-Myers Squibb, who currently dominate the chronic myelogenous leukemia (CML) treatment market, remains to be watched.