- LOGIN
- MemberShip
- 2025-12-21 15:08:34
- Policy
- Will Opdivo soon be reimb as first-line gastric cancer Tx?
- by Lee, Tak-Sun Aug 17, 2023 05:29am
- Whether Ono Pharmaceutical Korea’s ‘Opdivo Inj’ will receive reimbursement as the first first-line immunotherapy option for gastric cancer is gaining attention. If the drug is reimbursed as a first-line treatment for gastric cancer, Opdivo Inj may closely chase the sales of Keytruda, which had expanded coverage as a first-line treatment for non-small cell lung cancer in the immuno-oncology drug market. Three doses of Opdivo Inj were included in the updated list of drugs for which drug price negotiations were recently completed by the National Health Insurance Service. The list contains all the drugs that have completed pricing negotiations by the 10th of this month. After being recognized for the adequacy of reimbursement as a first-line treatment for gastric cancer by the Health Insurance Review and Assessment Service in May, the company has been negotiating the insurance drug price with the NHIS. Its reimbursement standards had been established in June last year by HIRA’s Cancer Disease Deliberation Committee (CDDC). The CDDC set the drug eligible for reimbursement as first-line treatment in combination with fluoropyrimidine- and platinum-containing chemotherapy for advanced or metastatic gastric cancer, gastroesophageal junction cancer, and esophageal adenocarcinoma. The analysis is that if the negotiations are complete, Opdivo will likely be listed for reimbursement soon after reporting to the Health Insurance Policy Deliberative Committee. In particular, HER2-negative gastric cancer, which Opdivo targets, accounts for nearly 90% of all patients. Therefore, the reimbursement expansion is expected to increase its sales greatly. Currently, Opdivo is reimbursed as monotherapy for 4 indications: as first-line and later lines of monotherapy for melanoma, as second-line and later lines of monotherapy for non-small cell lung cancer, as third-line or later lines of monotherapy for Hodgkin lymphoma, and as second-line or later lines of monotherapy for head and neck squamous cell carcinoma. Also, the drug is reimbursed in combination with Yervoy as a first-line treatment for renal cell carcinoma. Last year, Opdivo’s sales based on IQVIA sales was KRW 109.9 billion. Among immuno-oncology drugs, Opdivo recorded the second-highest performance after Keytruda (KRW 239.5 billion). Keytruda's sales have improved significantly compared to other immuno-oncology drugs after being granted reimbursement extensions as a first-line treatment for non-small cell lung cancer in March last year. If Opdivo also is granted a reimbursement extension as a first-line treatment for gastric cancer, it may also enjoy as explosive sales growth comparable to Keytruda.
- Policy
- ₩176.5 bil was spent on atopic dermatitis every year
- by Kim, Jung-Ju Aug 16, 2023 05:37am
- The National Health Insurance medical expenditures spent by patients with atopic dermatitis have risen every year to record KRW 176.5 billion last year. This is a 114.4% rise in 5 years. By age group, patients in their 20s accounted for 34.1% of the total expenditures, followed by those in their 30s (18.9%), then those in their 40s (11.8%). The National Health Insurance Service analyzed the NHI treatment data for atopic dermatitis from 2018 to 2022 using NHI data. The number of patients who received treatment for atopic dermatitis had increased from 92,0487 to 971,116 (5.5%↑), at an average annual increase rate of 1.3%. The number of male patients increased by 0.5% (1982↑) from 438,756 in 2018 to 440,738 in 2022, and female patients increased by 10.1% (48,647↑) from 481,731 in 2018 to 530,378 in 2022. Atopic dermatitis patients by gender (2018-2022) Looking at the composition of the number of patients treated for atopic dermatitis by age group, the most number of patients treated were 9 years old or younger, accounting for 28% (271,613) of all those treated in 2022 (971,116). Those in their 20s accounted for 16.7% (161,711), followed by teenagers accounting for 15.5% (150,837 people). Among male patients, those under the age of 9 accounted for the highest proportion (32.3%), followed by those in their teens (17.3%), then those in their 20s (16.4%). Among female patients, those under the age of 9 accounted for the highest proportion (24.4%), followed by those in their 20s (16.8%), then those in their teens (14.0%). When looking at the number of patients with atopic dermatitis per 100,000 population by year, the number rose from 1,802 in 2018 to 1,889 in 2022 (4.8%). Health insurance treatment costs for patients with atopic dermatitis increased by 114.4% (94.2 billion won) from 82.3 billion won in 2018 to 176.5 billion won in 2022, with an average annual increase of 21%. NHI expenditures spent to treat atopic dermatitis increased by 114.4% (KRW 94.2 billion) from KRW 82.3 billion in 2018 to KRW 176.5 billion in 2022, at an average annual increase of 21%. As of 2022, when looking at the proportion of NHI medical expenditures spent on patients with atopic dermatitis by age, those in their 20s accounted for the most at 34.1% (KRW 60.2 billion), followed by those in their 30s with 18.9% (KRW 33.3 billion) and those in their 40s with 11.8% (KRW 20.8 billion). By gender, both males and females in their 20s accounted for the most, accounting for 37.2% (KRW 40.3 billion) and 29.1% (KRW 19.9 billion), respectively.
- Policy
- Will it be possible to cover 'obesity drugs'?
- by Lee, Jeong-Hwan Aug 16, 2023 05:37am
- Attention is focusing on whether health insurance coverage standards for obesity treatment drugs, which are classified as non-reimbursed drugs that are not covered by health insurance, can be established. The Ministry of Health and Welfare announced that it had started discussions with the Korean Society of Obesity to discuss the necessity of reimbursement for obesity treatment and treatment and a reimbursement model to solve the problem of the domestic obesity rate. However, specific details, such as when and which obesity treatment and treatment will be applied, have yet to be confirmed. On the 14th, the Ministry of Health and Welfare submitted such a plan to the National Assembly regarding the reimbursement of medical treatment and treatment to solve the domestic obesity rate. The Health and Welfare Committee of the National Assembly requested the Ministry of Health and Welfare to unify the BMI (Body Mass Index) standard, which is the criterion for determining obesity and urged policies related to the introduction of drug treatment and reimbursement of obesity prevention medical services for severely obese people with a BMI of 30 kg/㎡ or more. Currently, the Ministry of Food and Drug Safety has changed the approval requirements and safe use standards for narcotic appetite suppressants to a BMI of 30 kg/㎡ or higher, but the Ministry of Health and Welfare has yet to establish a unified standard for obesity. The Ministry of Health and Welfare explained that in order to solve this problem, a meeting was held to discuss the need for unification of obesity BMI standards and the direction of adjustment. However, it was added that the need for further discussion was confirmed due to differences in opinions on key considerations such as the appropriate BMI standard for obesity, risk of death, risk of disease, life expectancy, and healthy life span. The Ministry of Health and Welfare plans to continue conducting additional reviews on the necessity and direction of the unification of obesity standards in the future. The Ministry of Health and Welfare announced that it would seek solutions together with academic societies regarding the payment of obesity treatment and treatment drugs. The Society for Obesity pointed out that there are frequent cases in which obese patients stop prescribing drugs due to economic burden through a 'survey on awareness and status of obesity treatment' last year, and emphasized reimbursement. Drugs used to treat obesity have obtained market approval from psychotropic narcotic drugs to GLP-1 analogs modified for diabetes treatment. Currently, in the case of obesity treatment, all treatments and medications except for surgical treatment for extremely overweight and extremely obese patients are not covered. The Ministry of Health and Welfare said, "We are discussing the necessity of reimbursement for obesity treatment and the reimbursement model with the obesity society."
- Policy
- In order to activate new drugs & raw materials in Korea
- by Lee, Tak-Sun Aug 11, 2023 05:36am
- Opinions were suggested that in order to further promote domestically developed new drugs and domestically produced raw materials, preferential drug prices are necessary. For new drugs developed domestically, the additional system should be used more actively and reference prices should be given to support exports. In order to increase the 20% level of self-sufficiency in raw material drugs, it is an opinion that the system of preferential drug prices for finished drugs using domestic raw materials should be revived. On the afternoon of the 9th, at the 'Policy Debate for the Advancement of the Global Center for Pharmaceutical Bio' (subtitle: Appropriate value of new drugs and measures to vitalize the raw material drug industry), co-hosted by Rep. Choi Jae-hyeong and the Korea Pharmaceutical Bio Association, domestically developed new drugs and raw materials were discussed. The need for a preferential plan for drug prices was raised. Park Gwan-woo, an attorney at Kim & Chang Law Office, who presented a plan to improve the reasonable drug price system for new drugs, argued for indirect support such as ▲ the introduction of an additional supplement system, ▲ expansion of the refund contract system, and ▲ tax benefits as measures to recognize the fair value of new drugs. He explained, "In the current drug price system environment, even new drugs belonging to the best-in-class are listed in the weighted average price method of alternative drugs, so it is not possible to attract additional research and investment." He went on to emphasize that “a virtuous cycle structure that leads to appropriate drug pricing, profit creation, and new drug development is needed.” "Considering the financial impact, trade issues, and drug pricing policy, it is necessary to expand the current addition system or refund contract system for innovative pharmaceutical companies," he said. "Indirect support such as tax benefits should also be considered." As with domestically developed new drugs, it is of the opinion that a preferential drug price system is necessary for domestically produced raw materials. Jung Yoon-taek, director of the Pharmaceutical Strategy Institute, said in a presentation on 'Domestic and International Trends and development plans for raw material pharmaceuticals', "The dependence on China and India is increasing, and the overseas dependence on domestic raw material pharmaceuticals is also increasing every year." He explained, "As of 2019, domestic self-sufficiency is 16.2%, and the domestic DMF ratio in 2020 is only 13.3%." He diagnosed that domestic pharmaceutical companies use imported APIs at a ratio of 9:1 to domestic APIs, indicating that imported APIs are already dominating the market. “The current drug pricing system gives 68% preferential treatment to generic drugs compared to original drugs for one year after launch when using our own synthetic ingredients,” said Director Jeong. He continued, "However, the problem is that generic drug price cuts have continued since the introduction of the lump sum drug price cut system in 2012, and the use of cheap overseas raw materials to lower manufacturing costs is increasing." Accordingly, it is explained that it is necessary to bring back the existing policy of preferential drug prices for drugs produced directly from raw materials, which was abolished in 2012. The panelists present on the day also supported the assertions of the presenters. Han Ssang-soo, chairman of the KPBMA Raw Materials and Drugs Committee, said, “Preferential drug prices for finished drugs using domestic raw materials is the most effective policy to increase the self-sufficiency rate.” did. Kim Ki-ho, managing director of HK Innoen, mentioned K-Cab, a new drug for gastroesophageal reflux disease that was approved in 2018, and said, "This drug has a competitive price in the global market as the 'preferential evaluation standard for domestically developed new drugs for global advancement', which was virtually abolished in 2018, is applied. , which helped us to advance overseas," emphasizing the need for preferential drug prices for domestically developed drugs through actual cases. At the end of the discussion, Oh Chang-Hyeon, manager of the Insurance Pharmaceutical Division of the Ministry of Health and Welfare, said, “We are currently in the process of coordinating while continuing to share opinions with the association during the first half of this year while promoting the improvement of the drug price system related to fair value compensation for innovative new drugs.” same," he said. "Basically, we are reviewing whether to recognize PE innovativeness, improving the listing process, and improving the follow-up management system," he said. He explained, “In the category of innovativeness, we try to include clinical superiority, innovative companies, whether or not to proceed with a rapid review for approval, and domestic R&D and clinical trials.” In addition, the improvement of the drug price system includes compensation for essential drugs in the health security sector, diversification of raw material supply and demand, and improvement of the drug price system for the stable supply of national essential medicines, said Manager Oh.
- Policy
- GPP drug Spevigo is first approved in Korea
- by Lee, Hye-Kyung Aug 11, 2023 05:36am
- The new orphan drug Spevigo (spesolimab) that is being imported by ‘Boehringer Ingelheim Korea has received domestic marketing authorization in Korea. The Ministry of Food and Drug Safety (Minister Yu-Kyung Oh) approved the new orphan drug Spevigo on the 9th. MoA of Spevigo Generalized Pustular Psoriasis (GPP) is characterized by systemic inflammation affecting the skin and internal organs. Its symptoms include diffuse erythema, fever, neutropenia, and skin pain. Spevigo is the first drug approved for GPP in Korea, and the drug is approved as a treatment for adult GPP patients who experience rapid worsening of their conditions. Spevigo is a humanized antagonistic monoclonal antibody that binds to the IL-36R. It prevents the subsequent activation of IL-36R and downstream activation of pro-inflammatory and pro-fibrotic pathways, providing a new treatment opportunity for GPP patients. The MFDS stressed that it will continue being committed to the rapid provision of safe and effective treatment options with verified safety and efficacy to expand treatment opportunities for patients with rare and intractable diseases based on its expertise in regulatory science.
- Policy
- PVG-004 succeeded in securing BA as the 1st generic K-CAB
- by Lee, Jeong-Hwan Aug 11, 2023 05:35am
- On the 10th, Pharmavision announced that the PVG-004 (Tegoprazan) project, which had transferred technology to SCD, succeeded in securing equivalence in the K-CAB and BA test for the first time in Korea. The reexamination expiration date (PMS) for K-CAB is July 4, 2024. Substance patents expire on August 25, 2031, and crystalline patents expire on March 12, 2036. Pharmavision and SCD adopted a strategy of parallel patent avoidance and BA test for rapid market launch and entry. Right after the PMS ends on July 4, 2024, with the goal of applying for marketing permission to obtain priority sales item rights, it is proceeding with a trial to avoid material patents and neutralize crystalline patents. Pharmavision co-CEOs Jin Jong-beom and Min Tae-kwon said, "With Pharmavision's formulation technology, we have secured the equality of K-CAB and BA tests for the first time in Korea or the world." We will grow together with customer pharmaceutical companies based on trust with a solution based on. Meanwhile, K-CAB's outpatient prescriptions in 2022 are about 125 billion won. It is a product with the third highest prescription amount among domestic prescription drugs, and the effect appears quickly after taking it. Currently, many domestic pharmaceutical companies are jumping into generic development.
- Policy
- 'Apply preferential pricing to non-inferior new drugs'
- by Lee, Tak-Sun Aug 11, 2023 05:35am
- With the government planning to release a drug price reform plan that includes a fair value compensation plan for innovative new drugs as early as next month, attention is focused on whether the reform will include a preferential measure for new drugs that demonstrate non-inferiority. This is because most of the new drugs that domestic pharmaceutical companies have successfully developed are new drugs that have demonstrated non-inferiority to existing drugs. Until now, non-inferior new drugs have been listed at a price below the weighted average of its alternatives. Therefore, the industry has been criticizing how the prices do not properly reflect the innovativeness of the developed new drugs. In addition, industry officials have pointed out that the low drug prices set in Korea render it difficult for companies to release their drugs overseas. To address this, domestic pharmaceutical companies have requested the government to provide additional scores for non-inferior new drugs as compensation while discussing the fair value of innovative new drugs. The government's policy on providing preferred measures for non-inferior new drugs was partially revealed on the 9th at the 'Policy Discussion for the Industry’s Leap to Become a Global Pharma & Bio Center (sub: Applying an Appropriate Value to New Drugs and Measures to Revitalize the API Industry)' that was co-hosted by Rep. Choi Jae-Hyung of the People Power Party and the Korea Pharmaceutical and Bio-Pharma Manufacturers Association. Director Chang-Hyun Oh from MOHW is discussing measures to compensate for the innovativeness of new drugs at a NA policy debate At the debate, Chang-Hyun Oh, Director of the Pharmaceutical Benefits Division of the Bureau of Health Insurance Policy at MOHW introduced, ▲clinical superiority, ▲innovative company designation status ▲expedited review subject status, and ▲domestic trial status as categories that the MOHW recognizes as innovative. Although Oh did not specify whether the clinical superiority of non-inferior drugs will be accepted, industry officials believe that this is highly likely. However, while explaining the point of Korea's positive listing system, Director Oh said that the current system’s structure does not provide preferential treatment to non-inferior new drugs and that he will work to take into account the pharmaceutical companies’ opinions to the extent that it would not jeopardize health insurance’s finances. An industry official who attended the event said, “Oh’s remarks may mean that only drugs that show clinical superiority can receive preferential treatment under Korea’s positive listing system and that non-inferior drugs are not subject to such treatment. However, the government also said it will consider reflecting the concept of an innovative new drug that was discussed by the public-private consultative body, such as taking into account the company’s innovative company status, domestic clinical trial status, MFDS expedited approval track status, etc., In that case, the non-inferiority criteria may not be important." Oh also added that the announcement was delayed due to the financial impact simulations the government conducted to assess the impact of the innovative new drug value compensation plan, and the results are likely to be released next month. The value of compensating non-inferior drugs was also emphasized by Gwan-Woo Park, a lawyer at Kim & Chang, who gave a presentation that day. Park, who had worked at the Health Insurance Review and Assessment Service for 4 years after graduating from Sahmyook University College of Pharmacy, said that most new best-in-class drugs that treat chronic conditions are being listed at 90% of the weighted average price of alternative drugs. Park said, “When a new drug for a chronic disease is released, it is difficult to convert the drug’s benefit into life expectancy extension or health-related life indicators required for QALY (quality-adjusted life year) calculation even if the drug has demonstrated clinical superiority. Therefore, a very low ICER (Incremental Cost-Effective Ratio) threshold is applied to those drugs. In particular, for indications that have generics drugs released, it is difficult for new drugs to obtain a price higher than that of the generics." Park explained that this was why most of the new drugs for chronic diseases are listed at 90% of the weighted average price of alternative drugs that were already listed for reimbursement. New drugs that were recently developed by domestic pharmaceutical companies are non-inferior drugs that target chronic diseases and are often listed at the weighted average price level of alternative drugs. On this, the pharmaceutical industry believes that for non-inferior new drugs to be properly valued, compensation should be provided so that the patients can receive the highest price of its alternatives.
- Policy
- Health insurance finance approved by the government alone
- by Lee, Jeong-Hwan Aug 11, 2023 05:35am
- It was pointed out again that health insurance finance should be included in the national finance and operated as a fund. There are concerns that if the health insurance finances are managed without going through deliberation by the National Assembly as it is now, transparency will be reduced and it can lead to negligence. The current method of independently reviewing and approving health insurance finances by the Ministry of Health and Welfare has also been criticized for being excessively discretionary and reducing the authority of health insurance subscribers. On the 10th, the National Assembly Budget Office announced this through an analysis of the Ministry of Health and Welfare’s financial statements for fiscal year 2022. Currently, health insurance finance is being operated through the health insurance general account of the National Health Insurance Corporation. The national pension, public servants pension, military pension, teacher pension, employment insurance, industrial accident compensation insurance, and long-term care insurance for the elderly are included in the national finance and operated as a fund. The Ministry of Budget and Policy considered it a problem that decision-making on health insurance finances was made without external control by the Health Insurance Policy Deliberation Committee, which was established and operated under the Ministry of Health and Welfare, and the Ministry of Health and Welfare approved NHIS accounting, budget, and settlement. It is unreasonable that the Ministry of Health and Welfare, which is the main body of health insurance policy establishment, has the right to review the budget and settlement of health insurance projects at the same time. The Ministry of Budget and Policy said that it is necessary to strengthen the National Assembly's control over the health insurance finance managed outside of the national finance, and to strengthen the transparency and accountability of financial operations. As a basis for this, it was said that national insurance premiums, which are the main financial source of health insurance finances, are in fact a quasi-tax, and that the government subsidizes a total of 20% of the expected income from health insurance premiums for that year, which causes limitations in figuring out the national fiscal balance. It pointed out the problem that if the increase in health insurance fiscal expenditure is not properly controlled, subscribers and the general public who pay insurance premiums and taxes will cover the cost. In particular, the National Fiscal Management Plan includes only a portion of the health insurance budget, which underestimates the scale of health and welfare expenditures and limits the ability to accurately grasp the actual total national expenditure. In addition, it was criticized that the health insurance policyholders' voting rights were not sufficiently guaranteed as the Ministry of Health and Welfare could take the lead in making decisions on major agendas related to health insurance finance input through a separate advisory meeting without deliberation and resolution by the Health Policy Deliberation Committee. During the deliberation on the calculation of the amount of compensation for losses in the medical sector caused by the promotion of reimbursement for ultrasound and MRI examinations, there were also cases where the Ministry of Health and Welfare did not provide enough data necessary for deliberation, such as reporting to the Health Policy Deliberation Committee on reduced profits in the medical sector. In response, the Ministry of Budget and Policy ordered the establishment of a health insurance fund, reconsideration of transparency in financial operations such as health insurance expenditure and income, and concrete measures to strengthen democratic control of the National Assembly, taking into account the characteristics and conditions of health insurance finances and the lack of a control function. The Ministry of Budget and Policy explained, “If the health insurance finance is operated as a fund, it is possible to operate it flexibly compared to the budget so that it can respond appropriately to the characteristics of short-term insurance.” Next, the Office of Budget and Policy pointed out, "Political issues in the National Assembly basically conform to the principle of representative democracy. The current decision-making structure rather exaggerates the scope of the government's discretion." “Expanding health insurance coverage and securing financial soundness is the premise and goal of health insurance finance operation, and the criticism that the expansion of coverage is hindered when funded is insufficiently grounded in logic,” he said.
- Policy
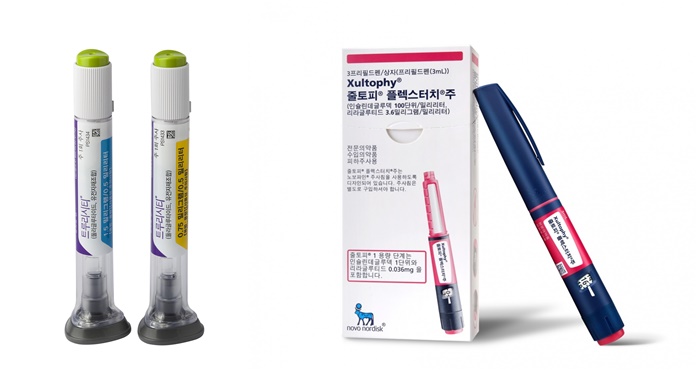
- Out of stock of GLP-1 injections
- by Moon, sung-ho Aug 10, 2023 05:33am
- As the news of GLP-1 (Glucagon-like peptide-1)-type diabetes treatments being used in clinical settings is reported one after another, concerns about this are growing. According to the medical community on the 4th, Novo Nordisk Pharmaceutical Korea is currently informing the clinical site of the out-of-stock news of Xultophy, a GLP-1 series diabetes treatment. Xultophy is a drug that controls blood sugar in adult type 2 diabetic patients and is a fixed ratio combination (FRC) of our company's basal insulin degludec and the GLP-1 analog liraglutide. After approval by the Ministry of Food and Drug Safety in Korea in 2019, it was applied as a benefit in May 2021 and is being used in clinical settings. However, due to the imbalance between demand and supply around the world, the aftermath also affected domestic clinical sites, resulting in out-of-stock products. The problem is that Lilly Trulicity, which was widely used as a GLP-1 diabetes treatment in domestic clinical settings prior to Xultophy, is also out of stock. In the clinical field, in the case of Trulicity out of stock, it is evaluated as the effect of concentration of production of Mounjaro, which is expected as a new drug for diabetes and obesity. A professor of endocrinology at general hospital A, who requested anonymity, said, "I heard that Xultophy may be out of stock soon after Trulicity. We inform patients in advance during treatment." The professor explained, "While checking the inventory status of the drugstore, some patients who were prescribed Trulicity are replacing it with DPP-4 inhibitor drugs." As a result, Soliqua is the only GLP-1 diabetes treatment that can be used as reimbursement in clinical settings. In the case of Xultophy, it can be replaced with Soliqua, but in the case of Trulicity, it is not easy to replace it with the corresponding treatment, the clinical field explains. Another professor of endocrinology at a tertiary general hospital who is an executive officer of the Korean Diabetes Association said, “There is no GLP-1 treatment that can be replaced with reimbursement for Trulicity, so the burden of non-reimbursement drugs will increase for patients. "For patients who are prescribed both insulin and Trulicity, Soliqua or Xultophy can be substituted, but there is no direct substitute for Trulicity," he pointed out. He said, “In this situation, as even Xultophy is out of stock, it seems that only Soliqua will be able to prescribe normally for the time being.” It is expected that the prescription of type 1 diabetes drugs will be disrupted." Meanwhile, current domestic and international diabetes treatment guidelines recommend preferentially considering GLP-1 injections, which have proven cardiovascular benefits, with SGLT-2 inhibitors in patients with atherosclerosis. Due to the high weight loss effect of GLP-1 injection, it is considered first in obese patients. Thanks to the guidelines, the domestic GLP-1 injection market, which is being applied as a benefit, is growing day by day. According to UBIST, a drug research institute, Trulicity recorded 54.7 billion won in sales last year, expanding its influence in the domestic clinical field. It recorded sales of 27.9 billion won in the first half of this year, continuing the upward trend of the previous year. Similarly, Xultophy recorded sales of 7.9 billion won in the first half of this year following the prescription record of 11.1 billion won last year. Soliqua is also showing sales growth, recording 6.3 billion won last year and 3.4 billion won in the first half of this year.
- Policy
- MOHW to expand ‘approval-assessment-negotiation’ project
- by Moon, sung-ho Aug 09, 2023 05:49am
- With the pilot project for the parallel operation of the ‘approval-assessment-negotiation linkage’ system that was implemented to shorten the drug reimbursement process in full swing, additional drugs are expected to be selected for the project in 2H this year. This is because the health authorities started a demand survey to select additional candidates for the pilot project in the second half of the year. Therefore, industry interest is rising on which items will additionally benefit. Pic. MOHW, HIRA, and NHIS have been operating the pilot project for the parallel operation of the ‘approval-assessment-negotiation linkage’ system this year According to industry sources on the 3rd, the Ministry of Health and Welfare, Health Insurance Review and Assessment Service, and National Health Insurance Service are planning to expand the operation of the ‘approval-assessment-negotiation linkage’ pilot project in 2H this year. The health authorities have been promoting a pilot project that included the parallel operation of the approval, benefit evaluation, and drug price negotiation system. The system was implemented to address the issue of how long and complicated the process for the reimbursement of high-priced rare diseases is. The authorities prepared a system that simultaneously operates the whole approval to reimbursement and drug price negotiation process. President Suk-Yeol Yoon had pledged to expedite the listing of ultra-high-priced drugs and expand reimbursement during his presidential campaign. Accordingly, the health authorities recently selected the neuroblastoma treatment Qarziba Inj (dinutuximab, Recordati) and the progressive familial intrahepatic cholestasis treatment advanced Bylvay (odevixibat, Ipsen) as priority candidates for its pilot project. Qarziba Inj, which is manufactured by the Italian pharmaceutical company Recordati, is being supplied by the Korea Orphan & Essential Drug Center in Korea. The drug is indicated for the treatment of high-risk neuroblastoma in patients aged 12 months and above. Bylvay is indicated for the treatment of pruritus in patients 3 months of age and older with progressive familial intrahepatic cholestasis. The drug received FDA approval in 2021. In Europe, the drug was approved to treat patients from the age of 6 months with progressive familial intrahepatic cholestasis. The French pharmaceutical company Ipsen had acquired Albiero which owns Bylvay earlier this year. The health authorities are now planning to select additional candidates for the project through a demand survey in 2H this year. The drug currently being discussed is 'Pluvicto (lutetium (177Lu) vipivotide tetraxetan), Novartis' prostate cancer drug. Also, Cablivi (caplacizumab), Sanofi's acquired thrombotic thrombocytopenic purpura (aTTP) treatment, is also being considered as a candidate. An industry official who requested anonymity, said, “The pilot project will be conducted in 2H 2023 to minimize the registration period for drugs that have proven superior treatment effects for patients with no appropriate treatment and a life expectancy of less than 1 year. The authorities will select candidates for the pilot project in 1H and carry out the project in 2H.” He added, “A demand survey may be conducted for Novartis’s ‘Pluvicto’ and Sanofi’s ‘Cablivi’ in 2H this year. The drugs subject to the project need to go through the MFDS’s Global Innovative products on Fast Track (GIFT), so the GIFT system is also being extended.”