- LOGIN
- MemberShip
- 2025-12-18 21:45:46
- Company
- Expanded competitiveness of K-Bio immunotherapies
- by Son, Hyung Min Aug 26, 2025 06:05am
- Korean pharmaceutical and biotech companies are entering the development of immunotherapies, increasing the possibility of 'big deals' with global pharmaceutical companies. As competition for new drugs targeting next-generation immune checkpoint proteins intensifies, Aprogen has begun developing VISTA targets by securing an antibody candidate from PharmAbcine. Companies such as Yuhan Corp, Hanmi Pharmaceutical, ImmuneOncia, and STCube are also implementing differentiated strategies with new target-based immunotherapies. Aprogen Secures PharmAbcine's Immunotherapy Candidate… 'Free supply agreement for Keytruda' According to the Financial Supervisory Service's electronic disclosure system on August 23, Aprogen recently secured an exclusive license for the research, development, and commercialization of the immunotherapy candidate PMC-309 through an agreement with PharmAbcine. Aprogen also obtained the rights for its manufacturing and production. The total contract value exceeds 10% of PharmAbcine's consolidated equity capital of KRW 47.7 billion as of last year, and the specific terms are undisclosed. The contract period runs from August 18, 2025, until the expiration of the final valid claim of the licensed patent. PMC-309 works by enhancing T-cell activity by blocking VISTA on the surface of immune T-cells and reducing the immunosuppressive function of myeloid-derived suppressor cells (MDSCs) to normalize the tumor microenvironment. This new drug candidate was discovered through PharmAbcine's fully human antibody library, 'HuPhage,' and specifically targets VISTA, a next-generation target for immunotherapy. A Phase 1 clinical trial of PMC-309 is currently underway in Australia. The Phase 1a part of the trial evaluates safety and pharmacokinetics with monotherapy, starting from low to high doses. The Phase 1b part will verify its combination effect with MSD's 'Keytruda.' MSD signed a free supply agreement for Keytruda with PharmAbcine in 2021, and this arrangement remains in effect for the current trial. The trial's patient enrollment goal is 67, with the first dose administered in November 2023. The expected completion date is 2028. Aprogen expects to see tumor shrinkage signals as early as the low-dose stage and anticipates a more pronounced anti-cancer effect at intermediate doses. Aprogen plans to quickly initiate the Keytruda combination Phase 1b trial once the target signals are confirmed at the intermediate dose, and to pursue early out-licensing to MSD if superior efficacy is proven in the combination therapy. Major Entry into Immunotherapy Market…All-Out Effort for Technology Transfer New antibody-drug conjugates (ADC)The immunotherapy development strategy of Korean companies can be summarized as 'signals,' 'speed,' and 'deal-making.' The structure involves securing meaningful response rates and safety data in the early clinical stage and using this as a basis to complete early technology transfers with global partners. This is why Korean companies are pursuing combinations with already commercialized immunotherapies or antibody-drug conjugates (ADCs). This Aprogen-PharmAbcine technology transfer deal is also notable for its collaboration with MSD, which opens the door for early technology transfer to a global pharmaceutical company. The industry is paying close attention to whether a major deal can be made when the clinical response rate, duration of response, and toxicity profile are disclosed. Currently, not only Aprogen and PharmAbcine but also Yuhan Corp, Hanmi Pharmaceutical, STCube, and GI Innovation are developing next-generation immunotherapies. Yuhan Corp recently received approval from the Ministry of Food and Drug Safety for its Phase 1/2 clinical trial plan (IND) for the bispecific antibody immunotherapy candidate 'YH32364.' YH32364 is a new drug candidate that Yuhan Corp in-licensed from ABL Bio in 2018. This trial is the first human dose study for YH32364. Yuhan Corp will evaluate the safety, tolerability, pharmacokinetics, and anti-tumor activity of YH32364 in patients with locally advanced or metastatic solid tumors that have confirmed overexpression of the epidermal growth factor receptor (EGFR). YH32364 is a bispecific antibody immunotherapy candidate that simultaneously targets EGFR and 4-1BB. Yuhan Corp plans to maximize the anti-tumor effect by simultaneously targeting EGFR, a biomarker expressed in major solid tumors like non-small cell lung cancer and colorectal cancer, and 4-1BB, which is involved in T-cell activation. Hanmi Pharmaceutical is conducting a Phase 1 clinical trial for its bispecific antibody immunotherapy candidate, 'BH3120.' BH3120 simultaneously targets PD-L1 and 4-1BB. As PD-L1 is a target where immunotherapies like Keytruda and Opdivo have proven their efficacy, Hanmi Pharmaceutical plans to enhance this effect by adding a 4-1BB protein target. GI Innovation recently changed its U.S. Phase 1/2 clinical trial for the immunotherapy candidate 'GI-102' to a study evaluating its combination therapy with Enhertu. GI-102 is a pipeline that targets CD80 and Interleukin (IL-2) to target tumor and immune cells. It has been engineered to have an even lower binding affinity to the alpha receptor compared to GI-101A. It is known that a high binding affinity to the alpha receptor increases regulatory T-cells, which reduces the anti-cancer effect. GI-102 is also being developed in a subcutaneous (SC) formulation, in addition to the intravenous (IV)formulation. The potential of GI-102 was also confirmed in a monotherapy trial. According to Phase 1/2a data recently disclosed by the company, GI-102 showed an objective response rate (ORR) of 43% in patients with melanoma. When GI-102 was administered, lymphocyte proliferation proceeded smoothly, and no serious drug toxicity was observed in terms of safety. GI Innovation anticipates a more pronounced effect when GI-102 is used in conjunction with Enhertu. The company believes that combining GI-102 with a reduced dose of Enhertu may decrease side effects, such as interstitial lung disease (ILD), which can occur with Enhertu. STCube is set to disclose the clinical results of 'Nelmastobart,' which targets the new biomarker BTN1A1. BTN1A1 is a protein that regulates the immune response to cancer cells by suppressing the activity of immune cells, T-cells. This biomarker is not expressed in normal cells but is strongly expressed in cancer cells, and its expression is mutually exclusive with PD-L1. ST Cube is developing an immunotherapy that targets BTN1A1, which could be a new treatment option for intractable cancers. ST Cube is currently conducting a U.S. and Korean Phase 1b/2 trial of Nelmastobart in combination with paclitaxel for patients with relapsed, refractory, and extensive-stage small cell lung cancer (ES-SCLC). The company is also investigating the potential of a Nelmastobart and capecitabine combination therapy as a third-line or later treatment for metastatic colorectal cancer. TiumBio recently disclosed the Phase 2 clinical trial results for its immunotherapy candidate 'TU2218' in combination with MSD's immunotherapy 'Keytruda.' TU2218 simultaneously blocks the pathways of transforming growth factor-beta (TGF-ß) and VEGF, which are known to inhibit immunotherapy activity, thereby maximizing the efficacy of immunotherapies. The disclosed trial represents the early cohort results from an ongoing study in patients with head and neck cancer and biliary tract cancer. The clinical results showed that the TU2218 + Keytruda combination therapy resulted in a partial response (PR) in 7 out of 11 patients with head and neck cancer, with stable disease (SD) observed in 1 patient. In the biliary tract cancer cohort, 4 out of 23 patients showed PR, and 7 showed SD. ImmuneOncia is conducting clinical trials for its immunotherapy candidate 'IMC-002.' IMC-002 has a mechanism that blocks signals between CD47 on cancer cells and macrophages. The recently disclosed results are the initial findings from an ongoing Phase 1b clinical trial in patients with hepatocellular carcinoma. The trial is evaluating the tolerability and safety of IMC-002 in combination with Lenvima, which is used to treat hepatocellular carcinoma. Among 10 patients who could be assessed for efficacy, the ORR was 30%, and the disease control rate (DCR) was 70%. The median time to progression (TTP) was 8.3 months.
- Company
- Jaypirca may be prescribed at general hospitals in Korea
- by Eo, Yun-Ho Aug 26, 2025 06:04am
- The BTK inhibitor Jaypirca may now be prescribed in general hospitals in Korea. According to industry sources on the 22nd, Lilly Korea’s relapsed and refractory mantle cell lymphoma treatment Jaypirca (pirtobrutinib) has passed review of Drug Committees (DCs) at medical institutions in Korea, including Samsung Medical Center, Pusan University Yangsan Hospital, and Ulsan University Hospital. As the company is currently in the final stages of price negotiations for Jaypirca with the National Health Insurance Service, it is expected that if it successfully secures insurance reimbursement, it will be immediately prescribed on-site. The drug was approved last August by the Ministry of Food and Drug Safety as a monotherapy in adult patients with relapsed or refractory mantle cell lymphoma (MCL) who have previously received two or more treatments, including BTK inhibitors. Prior to its approval, there were no approved medications available for patients with relapsed or refractory MCL whose disease progressed after treatment with existing BTK inhibitors in Korea. Also, Jaypirca is the first and only reversible BTK inhibitor that has demonstrated clinical efficacy in patients with relapsed or refractory MCL following treatment with one or more BTK inhibitors. It also exhibits a 300-fold higher selectivity for BTK compared to most kinases (98%) included in preclinical studies. The study that became the basis of Jaypirca’s approval was the BRUIN Phase I/II clinical trial, which evaluated the clinical efficacy and safety of Jaypirca in adult patients with relapsed or refractory mantle cell lymphoma who had previously received treatment with one or more BTK inhibitors. In the primary analysis set (PAS) of 90 patients who had previously received one or more BTK inhibitors, the overall response rate (ORR) was 56.7%, with a median duration of response (DoR) of 17.6 months. The most common adverse reactions following Jaypirca administration were fatigue (26.3%), neutropenia (22.8%), diarrhea (22.1%), and bruising (19.0%). The incidence of treatment discontinuation due to adverse reactions was 1.2%, and the incidence of dose reduction due to adverse reactions was 3.3%. Meanwhile, based on the response rate results, Jaypirca was approved through the U.S. FDA's accelerated approval process in January last year. In Korea, it was designated as an orphan drug in June last year for use as monotherapy in adult patients with relapsed or refractory MCL who had previously received treatment with a BTK inhibitor.
- Company
- 'New treatment opportunities rise for acquired hemophilia A'
- by Whang, byung-woo Aug 25, 2025 06:06am
- There is an extremely rare bleeding disorder that affects one in every 100,000 people. It is acquired hemophilia A, a condition in which healthy individuals experience unexplained bruising and severe bleeding throughout the body. Until recently, there were limited treatment options available for emergencies, causing significant challenges for medical staff in controlling the patients’ bleeding. Episodes. In this context, the introduction of “Obizur ( susoctocog alfa), a blood coagulation factor VIII agent” as the first treatment for adult acquired hemophilia A in Korea last year, followed by its reimbursement, has brought about major changes in the treatment environment. Dailpharm met with Jin Seok Kim, Professor of Hematology at Severance Hospital, to discuss the changes brought about by the introduction of Obizur in clinical practice and the challenges that remain. Unexplained autoimmune bleeding…delayed diagnosis can be fatal Jin Seok Kim, Professor of Hematology at Severance Hospital While congenital hemophilia is a bleeding disorder caused by genetic factors, acquired hemophilia A occurs when antibodies against blood coagulation factor VIII (Factor VIII) are produced due to an autoimmune response. This rare disease causes bleeding by inhibiting the function of Factor VIII, and its symptoms appear similar to those of congenital hemophilia, such as bruising or bleeding. Professor Kim explained, “While acquired hemophilia can arise secondary to malignant tumors, autoimmune diseases, medications, or pregnancy, approximately 50% of cases are reported as idiopathic, meaning they occur without a clear underlying cause. Given its rarity and unfamiliarity, patients may feel overwhelmed, but some cases can progress to severe bleeding requiring emergency treatment, making prompt diagnosis critically important.” According to statistics from Western countries, the incidence is approximately 1 in 1 million people, which translates to about 50 cases per year in South Korea based on its population. However, the actual number of reported cases in the country is much lower, estimated at around 20 per year. Professor Kim added, “Since acquired hemophilia A is such a rare disease, general medical staff are often unaware of it, leading to delayed diagnosis. When treating patients with unexplained generalized bleeding or atypical bleeding patterns, it is crucial to actively work with a hematologist.” The primary goal of treatment for acquired hemophilia A is to stop life-threatening bleeding while removing antibodies to prevent recurrence quickly. This requires concurrent hemostatic therapy and immunosuppressive therapy, a process that is highly complex and challenging. Professor Kim explained, “Acquired hemophilia A requires not only hemostasis but also immunosuppressive therapy to remove autoantibodies, which can make treatment complex and risky. Highly potent immunosuppressants such as steroids and cyclophosphamide must be used to remove antibodies, but in elderly patients, the risk of severe infections such as pneumonia and sepsis is high, and death from infection during treatment is not uncommon.” Intoduction of Obizur changes the paradigm of acquired hemophilia A treatment There were also difficulties in selecting emergency hemostatic agents. Prior to the introduction of Obizur, bypassing agents were the standard hemostatic treatment for acquired hemophilia A. These are medications that bypass the deficient Factor VIII in the body and help form fibrin clots through an alternative pathway. In South Korea, recombinant activated Factor VII (rFVIIa, eptacog alfa) was primarily used as first-line therapy. rFVIIa activates blood clotting factors in a short time to induce temporary hemostasis, but it has the limitation of a very short duration of action (half-life) of approximately 2 hours. Professor Kim mentioned, “Due to its very short half-life of two hours, as well as the high cost of the drug and reimbursement limitations, it was difficult to adhere to the recommended dosing interval (two hours), resulting in insufficient hemostasis or recurrent bleeding in many cases.” In this situation, Obizur, which was reimbursed last year, is said to have brought a positive impact. Obizur is a recombinant porcine sequence factor VIII (rpFVIII) drug developed to avoid cross-reactivity with human factor VIII autoantibodies. It can replace factor VIII to achieve hemostatic effects and has a longer half-life of approximately 10 hours, enabling stable and sustained hemostatic management. Professor Kim stated, “It has been just over a year since Obizur was introduced. While we are still accumulating clinical evidence, experts on the front lines are clearly sensing positive changes. Obizur is evaluated as having equivalent hemostatic efficacy and effectiveness to existing bypass therapies, but with the ability to monitor treatment responses more objectively, which is a key differentiator.” When using existing bypass therapies, decisions on dose reduction or treatment termination were based solely on the patient's clinical bleeding signs. However, Obizur allows for objective determination of treatment dose and duration by measuring plasma factor VIII levels. He explained, "Once bleeding is controlled, treatment can be discontinued early based on numerical confirmation, and conversely, additional doses can be administered if levels do not rise sufficiently, enabling personalized treatment. This reduces unnecessary overdose and the risk of side effects such as thrombosis, and since only the optimal dose for each patient is used, the cost of treatment is also reduced.” Reimbursement standards still remain a barrier... “Clinical judgment should be taken into account in reimbursement decisions” Although the treatment environment for acquired hemophilia A has improved significantly with the introduction of Obizur, practical constraints and remaining challenges still do exist. One of the most notable issues is its health insurance reimbursement criteria. Currently, under Korea’s reimbursement standards, only patients with antibody titers of 5 BU or higher are eligible for reimbursement for bypass agents or Obizur, which is the same as for congenital hemophilia patients. However, experts believe that the current criteria, which require selecting medications based on antibody titers, are inappropriate for acquired hemophilia as there is a low correlation between antibody titers and bleeding severity. Professor Kim stated, “Under the current reimbursement criteria, it is necessary to confirm the antibody titer before starting treatment and determine insurance coverage, which can lead to treatment delays or administrative burdens. Additionally, the 5BU standard is not applied in any domestic or international treatment guidelines.” He further explained, “Even with low antibody titers, severe bleeding can occur in acquired hemophilia, so clinical manifestations may differ significantly even if test results are similar. Therefore, it is necessary to improve the system to determine insurance coverage based on the patient's bleeding patterns and clinical judgment rather than quantitative criteria.” In addition, Professor Kim emphasized the need to prompt early diagnosis by raising disease awareness. He explained, “Even if effective treatments exist, delayed diagnosis inevitably worsens prognosis, and ultimately, the success of treatment depends on how fast we diagnose the condition. Since acquired hemophilia is a rare disease, the general medical staff have low awareness, leading to delayed initial diagnosis. Improving disease awareness is essential to prevent deaths caused by severe bleeding in the early stages.”
- Company
- Lilly seeks Mounjaro’s reimbursement for diabetes in Korea
- by Eo, Yun-Ho Aug 22, 2025 06:08am
- ‘Mounjaro,’ which is causing a roar in the field of obesity treatment, is seeking inclusion in insurance reimbursement for its diabetes indication. According to Dailpharm coverage, Eli Lilly Korea has submitted a reimbursement application for its Mounjaro (tirzepatide), a dual GIP/GLP-1 receptor agonist, and is proceeding with the necessary procedures to present the application for review to the Drug Reimbursement Evaluation Committee of the Health Insurance Review and Assessment Service. Therefore, it remains to be seen whether Mounjaro, a drug for obesity and diabetes, will be listed for reimbursement in Korea. Mounjaro is a single-molecule designed to selectively bind to and activate the GIP receptor and GLP-1 receptor with a once-weekly injection. It helps lower blood sugar by promoting insulin secretion, improving insulin sensitivity, reducing glucagon levels, delaying stomach emptying, and reducing food intake, thereby aiding weight loss. Although its obesity indication is well-known, Mounjaro has achieved significant results in the field of diabetes as well. Beyond just achieving the blood sugar control targets, 6 out of 10 patients achieved normal blood sugar levels without an increased risk of hypoglycemia, reaching the ultimate treatment goals of preventing cardiovascular complications and reducing mortality. It has even demonstrated the potential for “remission” in diabetes. In diabetes, Mounjaro is approved as an adjunct to diet and exercise therapy for improving glycemic control in adults with type 2 diabetes (as monotherapy or as part of a two-drug regimen). The approval of its type 2 diabetes indication approval was based on a randomized, double-blind, placebo-controlled study comparing Mounjaro (5 mg, 10 mg, or 20 mg) with placebo, semaglutide (1 mg), insulin degludec (100 U/mL), and insulin glargine (100 U/mL) in five SURPASS Phase III clinical trials (total of 6,278 participants). Mounjaro significantly improved HbA1c compared to the control group and baseline in all studies. Meanwhile, the top-line results from the Phase III SURPASS-CVOT study, which demonstrated the cardiovascular benefits of Mounjaro, have recently been disclosed. In the study, Mounjaro demonstrated non-inferiority compared to Trulicity in the incidence of 3-point major cardiovascular events (MACE-3), including cardiovascular disease death, myocardial infarction, and stroke, thereby achieving the primary endpoint of the clinical trial. Additionally, it showed improvements in key outcomes, including HbA1c, weight, kidney function, and all-cause mortality.
- Company
- Leclaza at global crossroads 1 year into FDA approval
- by Moon, sung-ho Aug 22, 2025 06:06am
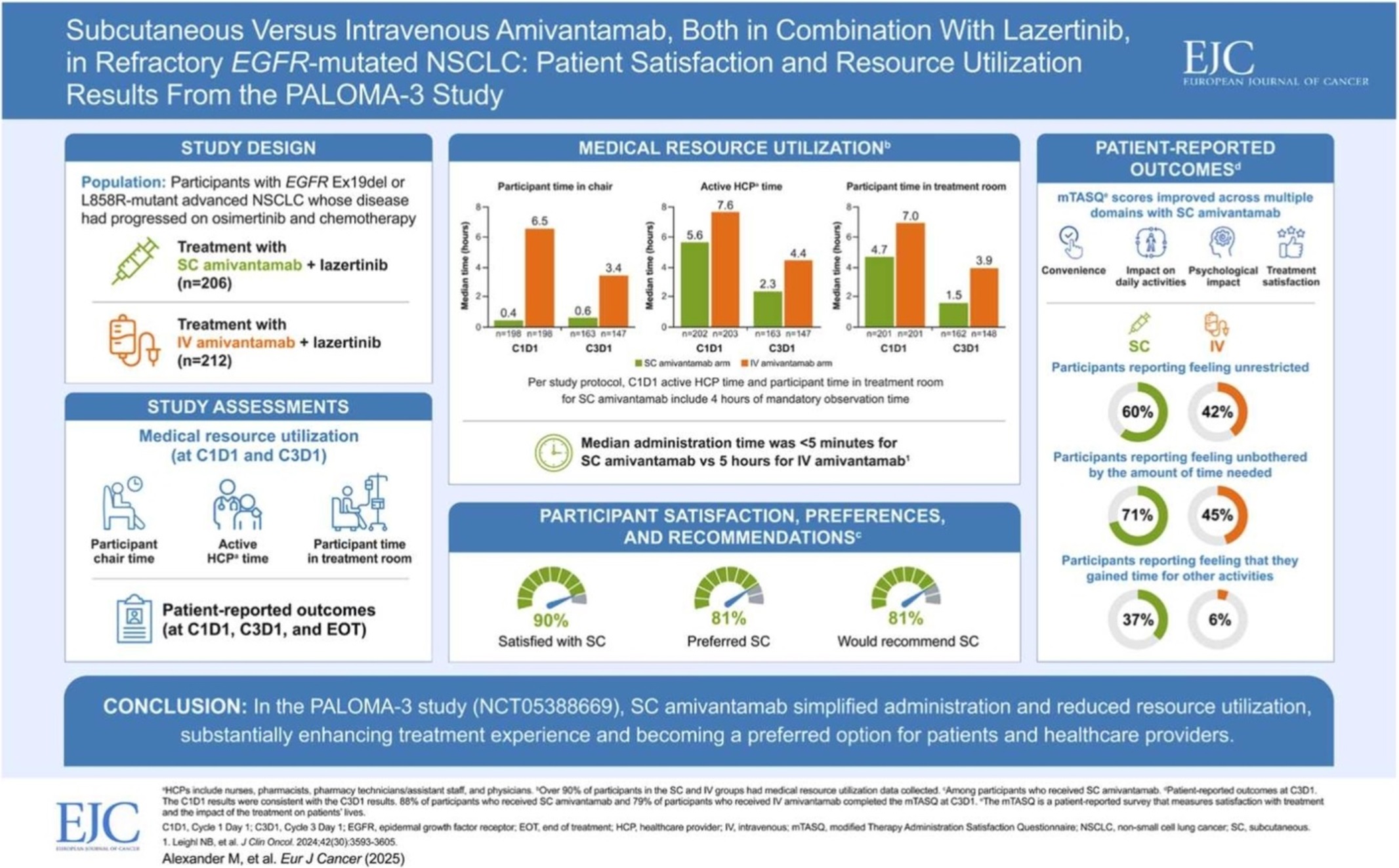
- One year has passed since Leclaza (lazertinib) received FDA approval in combination with Johnson & Johnson’s Rybrevant (amivantamab). Expanding its influence beyond the United States to Europe and Asia, it has emerged as a global treatment option both in Korea and abroad. In the first half of this year, it recorded an overall survival rate (OS) exceeding 50 months, emerging as a global standard of care for non-small cell lung cancer and contributing to a major shift in the treatment paradigm. # With the FDA’s decision on whether to approve Rybrevant SC set to be determined in the second half of this year, another 'step-up' is also anticipated for Leclaza, depending on the result. According to industry sources on the 18th, the FDA approved the use of Rybrevant in combination with Leclaza (US brand name: Lazcluze) as a first-line treatment for adult patients with locally advanced or metastatic non-small cell lung cancer (NSCLC) with EGFR exon 19 deletion or exon 21 L858R substitution mutation, or adult patients with locally advanced or metastatic non-small cell lung cancer (NSCLC). The combination was also approved in Europe in December of the same year, followed by the UK (March), Japan (March), and Canada (March) in the first quarter of this year, and China (July) in the second quarter. In May, prescriptions began in Japan, indicating the combination is gaining momentum in its expansion into the global market. Among the countries that have approved the combination, the combination’s performance in China is particularly noteworthy. With approximately 1 million new lung cancer diagnoses each year, lung cancer is the No.1 cancer in terms of incidence and mortality in China. This accounts for more than one-third of the 2.5 million new lung cancer cases worldwide. In addition, approximately 85% of lung cancer patients in China have non-small cell lung cancer (EGFR accounts for 40% of non-small cell lung cancer). Furthermore, the OS results of the Phase III (MARIPOSA) study presented at the European Lung Cancer Congress (ELCC 2025) held in Paris, France, in March this year have further accelerated the growth momentum. According to the Phase III MARIPOSA study, the combination therapy arm that received Rybrevant and Leclaza saw a 25% reduction in risk of death compared to the Tagrisso (osimertinib, AstraZeneca) arm (HR=0.75, 95% CI: 0.61–0.92, P
- Company
- Nubeqa gains flexibility with indication expansion
- by Whang, byung-woo Aug 21, 2025 06:06am
- The influence of Nubeqa (darolutamide) is rising in the market with the company expanding its indication as a treatment for metastatic hormone-sensitive prostate cancer (mHSPC). Experts believe that the drug may settle as a flexible treatment option in Korea’s market as it has broadened its path as a personalized treatment. With the approval, overcoming the reimbursement hurdles is expected to serve as the key to competition in the future. Hyun-ho Han, professor of Urology at Severance HospitalBayer Korea held a media seminar on the 20th to celebrate the indication expansion for Nubeqa, an oral androgen receptor inhibitor (ARi), and highlighted its clinical significance. In June, Nubeqa was approved by the Ministry of Food and Drug Safety as part of a two-drug regimen in combination with androgen deprivation therapy (ADT) for the treatment of metastatic hormone-sensitive prostate cancer (mHSPC). In South Korea, Nubeqa was previously approved for use in combination with ADT and docetaxel for the treatment of mHSPC patients, as well as in combination with ADT for the treatment of high-risk non-metastatic castration-resistant prostate cancer (nmCRPC). With the expanded indication, Nubeqa can now be used not only as a three-drug regimen in combination with ADT and the chemotherapy agent docetaxel but also as a two-drug regimen in combination with ADT. The approval was based on the results of the global Phase III clinical trial ARANOTE, which evaluated the efficacy and safety of the two-drug regimen of Nubeqa in combination with ADT in 669 patients with mHSPC. The study results showed that the Nubeqa combination group significantly reduced the risk of radiographic progression or death by 46% compared to the placebo group, and this improvement in radiographic progression-free survival (rPFS) was consistently observed across all groups, including high-risk and low-risk mHSPC patients. Also, in the secondary endpoint, overall survival (OS), the Nubeqa combination therapy group demonstrated potential survival benefits compared to the placebo group, showing significant delays in disease progression in terms of PSA level, deterioration in quality of life, and pain progression, thereby proving clinically meaningful improvements in quality of life. The most significant aspect of this expanded indication is that Nubeqa is now the only treatment approved for both three-drug regimens with docetaxel and two-drug regimens with ADT in patients with metastatic hormone-sensitive prostate cancer. The introduction of this new option is expected to offer a more flexible treatment approach tailored to the individual condition and treatment goals of mHSPC, including providing treatment options for elderly patients or those who are not suitable for chemotherapy. Hyun-ho Han, professor of Urology at Severance Hospital, who presented at the media seminar, said, “Most mHSPC patients in Korea are elderly, aged 60 or older, and often have comorbidities. It is necessary to devise personalized treatment strategies based on clinical evidence, taking into account the patient's condition and preferences.” Professor Han added, “With the approval of the two-drug Nubeqa + ADT regimen, it is now possible to tailor treatment according to patient characteristics depending on whether docetaxel is used. Patients who require aggressive initial treatment can consider the three-drug combination therapy of Nubeqa + ADT + docetaxel, while patients with CNS concerns, such as the elderly or those with chronic diseases, or patients who are not suitable for docetaxel treatment, can consider the two-drug combination therapy of Nubeqa + ADT." Currently, Nubeqa is approved in over 85 countries worldwide as a treatment for mHSPC and nmCRPC, and as of 2024, it has surpassed annual sales of approximately KRW 2.4 trillion, establishing itself as a blockbuster drug. However, it is still non-reimbursed in Korea, resulting in high costs and limited access for patients. Currently, treatments such as Xtandi, Zytiga, and Erleada are reimbursed as treatments for mHSPC, so reimbursement is essential for competition with these products.. On this, Professor Han emphasized that Korea needs more treatment options when considering the criteria set for reimbursement of the existing drugs in prostate cancer. He said, “There are cases when patients with metastatic prostate cancer or non-metastatic castration-resistant prostate cancer are not eligible for reimbursement coverage. We want to offer cost-effective choices to patients, so any additional covered option that are introduced are welcome on our part.” Considering that existing treatments can only be used in combination with ADT, Professor Han believes that the three-drug regimen of Nubeqa + ADT + docetaxel may offer additional advantages. In addition, MyungKyu Noh, Oncology BU lead at Bayer Korea, said, “Bayer Korea is going through the reimbursement process so that domestic prostate cancer patients can promptly receive our treatment and its reimbursement as soon as possible. We will actively communicate with various stakeholders, including patients, medical staff, and the government, to improve access to treatment for all three indications.
- Company
- Reimb of polycythemia vera drug 'BESREMi' likely in Sept
- by Eo, Yun-Ho Aug 21, 2025 06:06am
- The polycythemia vera treatment 'BESREMi' is expected to be listed on the national health insurance list. The National Health Insurance Service (NHIS) and PharmaEssentia Korea have recently reached a final agreement on the drug price negotiation for BESREMi (ropeginterferon alfa-2b). As a result, if it passes the Health Insurance Policy Review Committee, it can be officially listed in September. BESREMi's company had previously proceeded with the reimbursement process for hydroxyurea-refractory or intolerant polycythemia vera in March 2023. It failed to pass the Health Insurance Review & Assessment Service (HIRA)'s Cancer Disease Review Committee in July of the same year. At that time, the Cancer Disease Review Committeedetermined that there was insufficient evidence to judge the clinical utility of BESREMi as a second-line treatment. PharmaEssentia subsequently supplemented the evidence for this drug's efficacy as a second-line therapy by adding domestic clinical data. It resubmitted the reimbursement application in March of last year, passed the Cancer Disease Review Committee in July of the same year, passed the Drug Reimbursement Evaluation Committee in May, and has now completed the negotiation stage. BESREMii is a next-generation interferon that selectively eliminates the JAK2 mutant gene, which is the cause of polycythemia vera. It was developed to improve the purity and tolerability of existing interferons, allowing for once-every-two-week administration for the initial 1.5 years and once every four weeks thereafter. BESREMi is currently recommended in the National Comprehensive Cancer Network (NCCN) and European LeukemiaNet (ELN) guidelines for the treatment of polycythemia vera, regardless of prior treatment history. Meanwhile, polycythemia vera is a rare blood cancer in which a somatic mutation in the bone marrow abnormally activates bone marrow function, leading to excessive production of red blood cells. According to HIRA data, the number of prevalent patients in Korea is around 5,000, and hydroxyurea is primarily used for more than half of these patients. However, the currently reimbursed drugs are not a fundamental treatment. For patients who fail hydroxyurea treatment, there is no new alternative, making it a disease with high unmet needs.
- Company
- Viatris signs exclusive sales and distribution deal for Brid
- by Whang, byung-woo Aug 21, 2025 06:05am
- Pic of Bridion Viatris Korea announced on the 20th that it has signed an exclusive domestic promotion and distribution agreement for the general anesthesia reversal agent Bridion (Sugammadex) through a strategic partnership with MSD Korea. Under the agreement, Viatris Korea officially took over the domestic promotion and distribution of Bridion as of the 7th of this month Bridion is a general anesthesia reversal agent developed by MSD, which was approved by the Ministry of Food and Drug Safety in October 2012 and launched in Korea in February 2013. Over the past decade, Bridion has established itself as a treatment option that enables rapid and predictable muscle relaxation recovery in clinical settings. Through this strategic partnership, Viatris Korea plans to expand its product portfolio into anesthesia in Korea, enhance patients' access to treatment, and strengthen its market leadership by leveraging its robust sales and marketing capabilities in the general hospital sector. Bill Schuster, Country Manager of Viatris Korea, said, “We are very pleased to add Bridion, MSD's general anesthesia reversal agent that has made many innovative marks in the anesthetic field, to our portfolio. This agreement will further solidify the partnership between the two companies and enable us to better provide treatment access to patients in need of Bridion amid rapidly changing market conditions.” He added, “As a company that empowers people to live healthier lives at every stage of life, Viatris Korea will continue to strive to provide healthcare professionals and patients with more effective and safer treatment options.” Bridion is a rapid and predictable neuromuscular blocking agent reversal drug that selectively reverses the effects of rocuronium or vecuronium, neuromuscular blocking agents used during anesthesia. It completely reverses neuromuscular blockade within an average of three minutes, enhancing the safety and efficiency of anesthesia recovery. Albert Kim, Managing Director of MSD Korea, said, “We expect that surgeons and patients in Korea will be able to continue to benefit from Bridion through our exclusive agreement with Viatris Korea, a company with strong expertise in the field of chronic diseases. Based on our trusted partnership, both companies will do their utmost to ensure a stable supply of Bridion in Korea.”
- Company
- Generics challenge the patent of mkt leading 'Rinvoq'
- by Kim, Jin-Gu Aug 21, 2025 06:05am
- Product photo of Rinvoq The patent challenges by generics targeting AbbVie's Janus kinase (JAK) inhibitor' Rinvoq (upadacitinib)' have begun. The pharmaceutical industry anticipates that patent challenges will further expand as Rinvoq strengthens its monopolistic position in the JAK inhibitor market, which is valued at approximately KRW 62 billion annually. Chong Kun Dang Files Invalidation Trial for Rinvoq's Methods of Manufacture…More Companies Expected to Join According to the pharmaceutical industry on the 20th, Chong Kun Dang filed a petition for trial to confirm the scope of rights against AbbVie on the 19th regarding Rinvoq's manufacturing method patent. This is the first patent challenge against Rinvoq. Rinvoq is a JAK inhibitor used to treat autoimmune diseases, including rheumatoid arthritis and atopic dermatitis. Its mechanism of action inhibits the production of inflammatory cytokines, thereby blocking inflammation, pain, and cell activation. After Xeljanz was launched in 2015, Olumiant and Rinvoq joined the competition in 2019 and 2021, respectively. Cibinqo and Jyseleca joined in 2023. Rinvoq has two registered patents: a substance patent expiring in May 2032 and a method of manufacture patent expiring in October 2036. It is expected that companies will first circumvent the patent expiring in 2036 and then launch their generics early, around the time of the expiration of the substance patent in 2032. The pharmaceutical industry expects that more companies will challenge Rinvoq's manufacturing method patent, following Chong Kun Dang. This is because the JAK inhibitor market is experiencing rapid growth, and Rinvoq is strenthening its monopolistic position. JAK Inhibitor According to pharmaceutical market research firm UBIST, the outpatient prescription sales of JAK inhibitors in the first half of this year were KRW 38.6 billion. This represents a 40% increase from the previous year, compared to KRW 27.5 billion in the first half of last year. JAK inhibitors are showing rapid growth in the autoimmune disease treatment market, driven by the convenience of their oral formulation. The JAK inhibitor market, which was KRW 18.7 billion in 2020, grew by 36% to KRW 25.5 billion the following year. The market size expanded with the addition of Rinvoq in 2021. Subsequently, it grew significantly each year, reaching KRW 35.5 billion in 2022, KRW 40 billion in 2023, and KRW 62.2 billion in 2024. During this period, the reimbursement expansion of key products drove market growth. An analysis suggests that the growth rate accelerated further after October 2024, when inter-class switching between JAK inhibitors for rheumatoid arthritis was approved for reimbursement. Rinvoq Strengthens Market Monopoly…H1 Market Share at 43% While the market has expanded, Rinvoq has further strengthened its monopolistic position. In the first half of this year, Rinvoq's prescription sales reached KRW 16.7 billion, a 49% increase from KRW 11.2 billion in the same period last year. Although prescription sales for other major JAK inhibitors also increased, their growth was not as rapid as Rinvoq's. Olumiant, the second-leading product in the market, saw a 26% increase from KRW 8 billion in the first half of last year to KRW 10.1 billion in the first half of this year. Xeljanz grew by 3% from KRW 6.9 billion to KRW 7.1 billion. Cibinqo and Jyseleca recorded prescription sales of KRW 3.2 billion and KRW 1.6 billion, respectively, in the first half of this year. As of the first half of this year, Rinvoq's market share in the JAK inhibitor market reached 43%. Compared to its 19% market share in the first half of 2022, this represents a 24 percentage point increase in three years. At the same time, Rinvoq, which was the third-largest player after Olumiant and Xeljanz, rose to the top spot in the market from the first half of 2024. Quarterly Sales Performance of Major JAK Inhibitors (unit: KRW 100 million, source: UBIST). GREEN-Rinvoq, SKY BLUE-Olumiant, BLUE-Xeljanz The rapid increase in Rinvoq's prescription sales is attributed to its having the most indications in Korea. Rinvoq holds indications for: ▲rheumatoid arthritis ▲psoriatic arthritis ▲ankylosing spondylitis ▲atopic dermatitis (adults and adolescents aged 12 and older) ▲ulcerative colitis and ▲Crohn's disease. Competing drug Olumiant has indications for: ▲rheumatoid arthritis ▲atopic dermatitis (adults and children aged 2 and older) ▲alopecia areata and ▲polyarticular juvenile idiopathic arthritis (pJIA). Xeljanz has indications for: ▲rheumatoid arthritis ▲psoriatic arthritis and ▲ankylosing spondylitis. Cibinqo has secured an indication for atopic dermatitis in adults and adolescents aged 12 and older, while Jyseleca has indications for rheumatoid arthritis and ulcerative colitis. A variable in this market is the launch of Xeljanz generics. The Xeljanz substance patent is set to expire in November this year. The crystal form patent, which expires in 2027, has been overcome by generic companies through numerous invalidation and circumvention trials. This means that Xeljanz generics are expected to launch all at once after November this year. Currently, 58 companies have obtained product approvals for 67 generic items and are ready for launch. Xeljanz generics are expected to be launched simultaneously without priority sales rights. This is because generic companies' victories in invalidation trials led to the deletion of the listed patents, making it impossible to acquire priority sales rights.
- Company
- Expanded patent dispute over cancer drug 'Xtandi'
- by Kim, Jin-Gu Aug 20, 2025 06:22am
- Product photo of Xtandi The number of companies challenging the patent for Astellas' prostate cancer treatment, 'Xtandi (enzalutamide)', has expanded to six. Attention has been drawn to the fact that major pharmaceutical companies, such as Chong Kun Dang, Hanmi Pharmaceutical, and JW Pharmaceutical, have joined this latest patent challenge. According to the pharmaceutical industry on August 19, Hanmi Pharmaceutical filed a petition for trial to confirm the scope of rights against Astellas for Xtandi's composition patent on August 18. As a result, the total number of companies that have filed circumvention trials against Xtandi's composition patent has increased to six. Earlier, Alvogen Korea was the first to file the trial on the 1st of this month, followed by Chong Kun Dang, JW Pharmaceutical, GL Pharma, and Kuhnil, where all filed the same trial. The pharmaceutical industry is paying attention to the fact that major pharmaceutical companies, such as Chong Kun Dang, Hanmi Pharmaceutical, and JW Pharmaceutical, have successively joined this patent challenge. This is because there have not been many cases where major pharmaceutical companies have simultaneously challenged patents for anti-cancer drugs. Typically, there is a high preference for prescribing original anti-cancer drugs, especially in large hospitals. Domestic pharmaceutical companies, which have strong sales capabilities for chronic disease treatments in clinics, have been hesitant to challenge patents for anti-cancer drugs for this reason. Furthermore, even if they succeeded in a patent challenge and launched a generic, the profits generated were not significant, making major pharmaceutical companies even more reluctant. There have been cases of patent challenges for liver cancer treatments like 'Lenvima (lenvatinib),' 'Cabometyx (cabozantinib),' and breast cancer treatment 'Ibrance (palbociclib).' However, these were sporadic challenges primarily led by Boryung, which has a separate oncology business unit, or Samyang Biopharm, which specializes in the generic oncology business. In the case of the oncology drug patent, Hanmi Pharmaceutical was the only company challenging the 'Nexavar (sorafenib) patent.' Meanwhile, in the patent challenge for the prostate cancer treatment Xtandi, major pharmaceutical companies like Chong Kun Dang, Hanmi Pharmaceutical, and JW Pharmaceutical have successively filed trials. If they win this trial, generic competition is expected to intensify after the substance patent expires in June 2026. Xtandi is Astellas' prostate cancer treatment, protected by two patents: a substance patent that expires in June 2026 and a composition patent that expires in September 2033. The plan for the generic companies is to circumvent the composition patent, which expires in 2033, and then launch their generics early around the expiration of the substance patent in 2026. Astellas received approval for Xtandi Soft Cap in 2013. Last year, it added two dosages of Xtandi tablets. Xtandi competes with Janssen's 'Erleada (apalutamide)' and 'Zytiga (abiraterone)' in the first-line prostate cancer treatment market. Recently, 'Akeega (abiraterone·niraparib),' a new first-line treatment, was launched. Akeega is a drug that combines Zytiga with Takeda's Zejula (niraparib). Recent trends indicate that while Zytiga's sales are declining following the launch of generics, Xtandi and Erleada are on an upward trend. According to pharmaceutical market research firm IQVIA, Xtandi's sales increased by 1.9 times in four years, from KRW 23 billion in 2019 to KRW 43.2 billion in 2023. It is estimated to have generated sales of around KRW 50 billion last year.