- LOGIN
- MemberShip
- 2025-12-17 20:28:09
- Company
- Rising childhood obesity in Korea’s limited environment
- by Eo, Yun-Ho Sep 22, 2025 06:11am
- The need for active management of childhood and adolescent obesity is becoming increasingly emphasized, along with growing interest in the appropriate use of pharmacotherapy. According to the ‘2020 Clinical Practice Guidelines of the Korean Society for the Study of Obesity,’ childhood obesity treatment in Korea primarily focuses on lifestyle modification—including diet, exercise, and behavioral therapy—to maintain appropriate weight. However, when weight continues to increase and comorbidities remain uncontrolled, pharmacological and surgical therapies are recommended along with lifestyle modification. Currently, pharmacological treatment for obese adolescents aged 12 or older is applied very selectively, taking into account both obesity status and growth stage. Medications are recommended in cases such as ▲ adolescents with severe obesity accompanied by complications, ▲ those with a family history of cardiometabolic diseases such as type 2 diabetes, or ▲ those whose weight or complications cannot be controlled despite intensive diet and behavioral therapy. Recommended drugs include GLP-1 receptor agonists such as Saxenda (liraglutide) and Wegovy (semaglutide), the fat absorption inhibitor Xenical (orlistat), and the appetite suppressant combination Qsymia (phentermine/topiramate). ◆Obesity patients in need of pharmacotherapy increase among children and adolescents Following the outbreak of COVID-19 in 2020, school attendance and outdoor activities were restricted, leading to decreased physical activity compared to pre-pandemic levels and accelerating the spread of obesity among adolescents. Like adult obesity, childhood obesity is associated with a range of comorbidities, including hypertension, dyslipidemia, type 2 diabetes, non-alcoholic fatty liver disease, obstructive sleep apnea, polycystic ovary syndrome, and mental health disorders such as depression. In children with severe obesity, even more serious cardiometabolic diseases than myocardial infarction or arteriosclerosis have been reported. As a general principle, obesity treatment aims for about 10% weight reduction and maintenance. However, due to the rebound yo-yo effect, one-third to two-thirds of the lost weight is typically regained within one year, and over 95% is regained within 5 years. Therefore, if non-pharmacological interventions such as diet and exercise fail to achieve more than 5% weight reduction after 3–6 months, active pharmacotherapy should be considered. If no meaningful weight loss of at least 5% occurs within 3 months of medication use, a new treatment strategy should be planned. Ultimately, lifestyle modification remains the first-line treatment for childhood obesity. However, for patients who fail to achieve weight loss through this approach, pharmacotherapy may be the best option before considering bariatric surgery. Candidates for obesity pharmacotherapy include those with a BMI above the 95th percentile and weight-related comorbidities, or those with a BMI at least 120% of the 95th percentile, regardless of comorbidity status, who do not respond adequately to lifestyle modification. Specifically, the proportion of obese children and adolescents in Korea requiring pharmacological treatment is currently estimated at 2–3%, and is expected to gradually reach below 5% due to dietary and lifestyle changes. ◆Limited pharmacotherapy options and considerations regarding Qsymia The problem is that, unlike abroad, the range of obesity treatments available in Korea is highly limited. Officially, the only drugs approved for use in children and adolescents aged 12 and above are Xenical and Saxenda. Xenical reduces fat absorption in the body. Despite the convenience of being an oral medication, it is used only sparingly due to common side effects such as diarrhea, abdominal pain, and increased intestinal gas. In addition, because it reduces absorption of fat-soluble vitamins, patients must take a daily multivitamin containing these nutrients. The American Gastroenterological Association (AGA) even recommended against using Xenical in its 2022 clinical practice guidelines on pharmacological interventions for adult obesity, citing these adverse effects. Qsymia can be prescribed to children and adolescents in the U.S., but it is not approved in Korea because one of its components, phentermine, is contraindicated for use in patients under 16. However, Qsymia—a combination that contains topiramate—enhances anti-obesity effects while lowering the dosage of each component compared to monotherapy, thereby reducing side effects. It also has the advantage of requiring only once-daily administration, regardless of meals. Concerns about pediatric prescription mainly stem from safety, but accumulating research data continues to address this issue. Clinical pharmacology trials comparing phentermine and topiramate in adults versus adolescents have shown no significant differences in efficacy or safety between the two groups. The studies found that both agents exhibited similar pharmacokinetic characteristics in adolescents and adults. The type, frequency, and severity of adverse drug reactions, as well as discontinuation rates due to adverse events, were also comparable, indicating no major differences in safety or tolerability between the two groups. Professor Seung-Hwan Lee of Seoul National University Hospital’s Department of Clinical Pharmacology stated, “The dose–pharmacokinetic–pharmacodynamic–clinical response relationships for phentermine and topiramate are similar in adolescents and adults. Therefore, the same dosage and regimen can be applied to adolescents as in adults. The adverse reactions are generally not severe and can be managed through dose reduction or discontinuation.”
- Company
- "Long-term survival possible for urothelial carcinoma"
- by Son, Hyung Min Sep 22, 2025 06:11am
- The treatment landscape for urothelial carcinoma is changing rapidly. Various approaches, including immunotherapy, antibody-drug conjugates (ADCs), and chemotherapy combination therapies, have been introduced. However, significant reimbursement barriers still exist in clinical practice. Among these, Merck's Bavencio (avelumab) is the only first-line maintenance treatment with insurance reimbursement applied in Korea. This drug has been a key treatment regimen of the long-term treatment strategy. In the JAVELIN Bladder 100 study, the basis of approval, Bavencio more than doubled overall survival (OS) compared to the prior standard of care, presenting a new paradigm that moved beyond a 'watch-and-wait' strategy. The latest real-world data (RWD) confirmed the clinical study, strengthening Bavencio's reliability in actual treatment settings. With most urothelial carcinoma patients being older adults, cost-effectiveness and safety are crucial for long-term treatment strategies. Experts' main opinion is that Bavencio is a treatment that satisfies both conditions simultaneously. DailyPharm met with Professor In Ho Kim of Seoul St. Mary's Hospital's Department of Medical Oncology and Professor Hongsik Kim of Chungbuk National University Hospital's Department of Hematology and Oncology to discuss the changes in the urothelial carcinoma treatment landscape and the reasons why the focus should be on long-term treatment strategies beyond just survival. Long-term survival effect confirmed by real-world data Both experts cited the consistent results of Bavencio, as demonstrated in RWD, as its greatest strength. RWD from multi-national studies, including the Japanese JAVEMACS, U.S. PATRIOT-II, and French AVENANCE trials, showed a median OS for Bavencio of over 30 months, with some analyses reporting extended results of over 40 months. Notably, a treatment strategy that continues with an ADC (such as enfortumab vedotin) after first-line Bavencio maintenance treatment has been reported to show an OS of over 41 months, substantially expanding the possibility of long-term survival for patients. Professor In Ho Kim of Seoul St. MaryProfessor Kim said, "In a clinical practice, it's very rare for a patient not to undergo Bavencio maintenance treatment. Except for a few patients who have difficulty adapting to immunotherapy, most are being treated with Bavencio maintenance therapy." Professor Kim added, "It is difficult for clinical trial data to become part of actual patient care, but Bavencio is an exception. The results from the clinical setting and the real world are almost identical." He assessed that "this drug provides a foundation for patients to continue treatment for a long time without difficulty." Professor Kim emphasized, "Because Bavencio has only a few side effects, it allows patients to continue therapy. Since patients feel comfortable with Bavencio maintenance treatment, long-term treatment is possible," and noted, "In clinical practice, patients are often in poorer health or are older than those in clinical trials, so we believe Bavencio's biggest advantage is that it can be used to treat these patients without difficulty." Data from Korea also supported these findings. An analysis of an Expanded Access Program (EAP) involving 30 patients from five Korean hospitals from 2021 to 2023 showed a median progression-free survival (PFS) of 7.9 months from the start of Bavencio, surpassing the 5.5 months in the JAVELIN Bladder 100 study. The complete response (CR) rate was 20%, and the median duration of CR reached 17.8 months. The fact that the results were consistent with global outcomes despite unfavorable conditions, 67% of patients were Stage 4 at diagnosis, and 40% had visceral metastasis, is highly significant. This also serves as the reason why Bavencio quickly became the standard of care for first-line maintenance therapy for urothelial carcinoma after its reimbursement application. Professor Kim said, "Clinical trials mainly include young, healthy patients, but in real-world practice, the majority of patients are older adults, with an average age of over 70." He added, "It is significant that the same survival curve appeared in this patient population as in the clinical trials." And he added, "Because Bavencio has few side effects, even patients in their mid-80s can use it without burden. When patients transition from platinum-based chemotherapy to Bavencio maintenance treatment, most see their condition improve after treatment, allowing them to proceed to second-line treatment, and there are many cases of long-term survival. The positive results confirmed in clinical trials are being directly translated into patient treatment." Professor Kim also mentioned, "In clinical settings, the effect was maintained even in patients with chronic kidney disease who were on dialysis. It has been confirmed that Bavencio maintenance treatment significantly improved patients' quality of life." First-line maintenance treatment as a practical alternative to reimbursement barriers While the number of urothelial carcinoma patients is steadily increasing in Korea, the treatment environment remains challenging. The recurrence rate after platinum-based chemotherapy is high, and immunotherapy as a monotherapy is not guaranteed to extend survival in the long term. Currently, various options are available for first-line urothelial carcinoma treatment. For example, combination therapies with immunotherapy and ADCs, as well as combination therapy with nivolumab + GemCis (gemcitabine + cisplatin). However, the ADC combination therapy is not covered by reimbursement, and the nivolumab and GemCis combination therapy is only reimbursed for a limited number of drugs. Bavencio maintenance therapy is currently the only option with reimbursement in Korea and is the most widely used in real-world clinical practice. Professor Hongsik Kim of Chungbuk National University HospitalProfessor Kim said, "Because I work at a regional hospital, I prioritize minimizing the financial burden on patients. I prefer treatments that are covered by reimbursement for long-term use. Consequently, we most often use gemcitabine-based platinum chemotherapy, followed by Bavencio maintenance treatment. If the disease progresses after Bavencio maintenance therapy, we use treatments like paclitaxel." He added, "On the other hand, for treatments like ADC, there isn't enough long-term sequencing data. Among the treatments currently used for urothelial carcinoma, Bavencio has the most abundant sequencing data, which provides a foundation for patients to receive stable Bavencio maintenance therapy for a long time in a clinical setting." The experts commonly pointed out that the future treatment paradigm should shift beyond simple life extension to a 'long-term treatment strategy.' Professor Kim explained, "What is particularly noteworthy in the urothelial carcinoma treatment landscape is that the number of second-line and later treatment options has increased significantly compared to the past. While immunotherapy monotherapy dominated in the past, a variety of new treatments have emerged, giving patients many more choices. I think this is a very fortunate change in the clinical setting." He continued, "With other immunotherapies and new drug candidates accumulating clinical evidence, a reimbursed first-line maintenance therapy is the most practical alternative for patients. Like other immunotherapies, Bavencio has a two-year limit on reimbursement. This drug can be administered for a long time until intolerance occurs. I understand the intent of the system, but since many patients remain stable for more than two years, I believe a separate discussion is needed based on individual patient circumstances." Finally, Professor Kim added, "Since Bavencio became reimbursed, many patients have had fewer worries during their treatment. Patients often place more value on a treatment-providing environment than on the drug itself. While various new drugs are being developed, I believe Bavencio will continue to play an important role in the urothelial carcinoma treatment."
- Company
- NMOSD patients call for Ultomiris’s reimbursement
- by Hwang, byoung woo Sep 22, 2025 06:11am
- With the emergence of an innovative treatment option for neuromyelitis optica spectrum disorder (NMOSD), a disease in which even one relapse can cause a dramatic decline in quality of life, voices are growing for improved access. Specifically, voices are rising on the need to improve access to Ultomiris (ravulizumab), which has demonstrated a relapse-free period of 73.5 weeks in a clinical trial, as a paradigm-shifting therapy to overcome the limitations of existing treatments. Need for treatment approaches focused on “relapse prevention” highlighted in NMOSD NMOSD is a central nervous system autoimmune disorder that causes nerve damage, primarily presenting with optic neuritis and myelitis. More than 90% of patients experience relapses. Neuromyelitis optica spectrum disorder (NMOSD) can lead to cumulative nerve damage with repeated relapses, potentially resulting in lower body paralysis or blindness.Repeated relapses lead to cumulative nerve damage, resulting in symptoms such as ocular pain, vision loss, spinal or limb pain, muscle weakness, gait disturbance, and sensory-motor impairment of the lower body, which may progress to paraplegia or blindness. NMOSD occurs most frequently in women in their 30s and 40s, an age group typically active in the workforce, leading to social isolation caused by employment discontinuation, reduced interpersonal interactions, and limited activity. This has negative repercussions not only on the individual but also on families and society as a whole. For example, patient A first experienced symptoms around the age of 16, but it took 5 years to receive an accurate NMOSD diagnosis. By then, despite devoting herself to treatment, the aftereffects of frequent relapses left her with significant daily limitations. She is currently being treated with MabThera (rituximab), but side effects make even basic tasks such as eating and walking difficult without family assistance. Long-term immunosuppressive therapy has also weakened her immunity, making her prone to colds, pneumonia, and enteritis, and at times she has faced emergencies such as breathing difficulties and shock. In NMOSD treatment, the key is to block relapses at an early stage. Experts in Korea and abroad emphasize that because even a single relapse can cause irreversible damage, treatment approaches aimed at preventing relapse itself are critical. Ultomiris demonstrates “relapse-free” effect in NMOSD Against this backdrop, the next-generation C5 complement inhibitor Ultomiris has gained attention as an innovative therapy, confirming relapse-free efficacy in a Phase III trial with NMOSD patients. By improving its half-life, the drug overcomes limitations of previous therapies, and among 58 patients in the Ultomiris group, the relapse rate during the trial period was 0%, suggesting a paradigm shift in NMOSD treatment. Pic of Ultomiris In the Phase III CHAMPION-NMOSD study, Ultomiris showed no relapses during a median treatment period of 73.5 weeks and reduced relapse risk by 98.6% compared to placebo. Dosing intervals are also noteworthy: Ultomiris can be administered every 8 weeks, significantly reducing treatment burden compared to Soliris, which requires dosing every 2 weeks. Professor Ho-Jin Kim from the Department of Neurology at the National Cancer Center explained, “The extended dosing interval not only reduces hospital visits, it also lowers physical strain and additional costs associated with travel for patients with impaired mobility and vision. Such improvements in treatment convenience can enhance patients’ quality of life and adherence to therapy.” However, the fact that Ultomiris is yet to be reimbursed in Korea limits actual treatment access. Accordingly, both clinical experts and the Korean NMOSD Patient Association are increasingly calling for guaranteed access to proven therapies. Patient A said, “I live with daily anxiety, never knowing when a relapse will strike. I know there is a therapy that prevents relapses, but cannot try it because it is not reimbursed.” Meanwhile, to promote proper understanding and social awareness of NMOSD, a “Stay ZERO” concert will be held on September 25 at the National Assembly Member Office Building. The event aims to amplify the voices of patients longing for a “relapse-free life,” raise awareness of the importance of relapse-prevention treatment, and emphasize the need for improved treatment accessibility.
- Company
- Reimb discussions begin for No.2 GIFT drug Nefecon
- by Eo, Yun-Ho Sep 22, 2025 06:10am
- Reimbursement discussions have begun for Nefecon (budesonide), the second drug designated under Korea’s GIFT (Global Innovative products on Fast Track) program and the first treatment for IgA nephropathy. According to industry sources, the Health Insurance Review and Assessment Service (HIRA) is expected to soon begin evaluation of the reimbursement application submitted late last year by Everest Medicines Korea. The specific indication under review is “treatment of adult patients with primary IgA nephropathy (immunoglobulin A nephropathy, IgAN) who have a proteinuria level of ≥1.0 g/day (or urine protein-to-creatinine ratio ≥0.8 g/g).” Nefecon was designated as the second GIFT drug by the Ministry of Food and Drug Safety (MFDS) in November 2024. With GIFT No. 1, Bylvay (odevixibat), essentially granted reimbursement, attention is now gathering on whether Nefecon will also be added to the reimbursement list. IgA nephropathy is an autoimmune glomerulonephritis in which immune complexes deposit in the glomeruli, causing chronic inflammation and kidney damage. Among severe patients with high proteinuria and low glomerular filtration rate, approximately 50% progress to ESRD (end-stage renal disease) or death within three years. Even after kidney transplantation, recurrence occurs in 20–60% of patients, severely impacting survival and quality of life. Until now, treatment has primarily involved conservative approaches such as RAS (renin–angiotensin system) inhibitors to control blood pressure, with dialysis or kidney transplantation considered only after significant renal function decline. This represents a major unmet need. The active ingredient in Nefecon, budesonide, is already marketed in Korea. Similar to antibody-drug conjugates (ADCs), which are targeted anticancer drugs designed to deliver cytotoxic anticancer agents used in chemotherapy to only the target site—cancer cells—thereby improving efficacy and safety, this is a targeted therapy designed to target Peyer's patches in the ileum, the final part of the small intestine. The initial stage of IgA nephropathy is the production of Gd-IgA1 (galactose-deficient IgA1). Since Gd-IgA1 is primarily produced in the Peyer's patches of the ileum, Nefecon targets this. In other words, it is designed to fundamentally treat the cause of IgA nephropathy by reducing the production of Gd-IgA1, the causative agent of the disease. This is also why regulatory agencies such as the US FDA, European EMA, China NMPA, and MFDS designated Nefecon for accelerated review and granted expedited approval. In a global Phase III clinical trial, 9 months of Nefecon treatment reduced kidney function loss by 50%, with similar effects observed after two years of follow-up. Data presented at ASN 2023 further projected that 9 months of Nefecon therapy could delay the need for dialysis by 12.8 years. Jin-hyang Jeong, Secretary-General of the Korea Organization for Rare Diseases, stated at a policy forum hosted on the 19th by lawmaker Ji-a Han of the People Power Party, “In Korea, IgA nephropathy patients are typically diagnosed at an average age of 34, in their prime working years. They face the lifelong risk of dialysis or kidney transplantation.” Jeong added, “Rather than spending the budget to maintain patients after renal function is lost, it is far more cost-effective to intervene earlier to prevent kidney damage. Special reimbursement coverage should be applied for severe IgA nephropathy patients.” Meanwhile, Nefecon received its first global approval from the U.S. FDA in December 2021 under the brand name Tarpeyo as the first and only approved treatment for IgA nephropathy. In Europe, it was conditionally approved in July 2022 under the brand name Kinpeygo and received full approval in July 2024. As of September 2025, Nefecon is reimbursed in the U.S., U.K., Italy, and China.
- Company
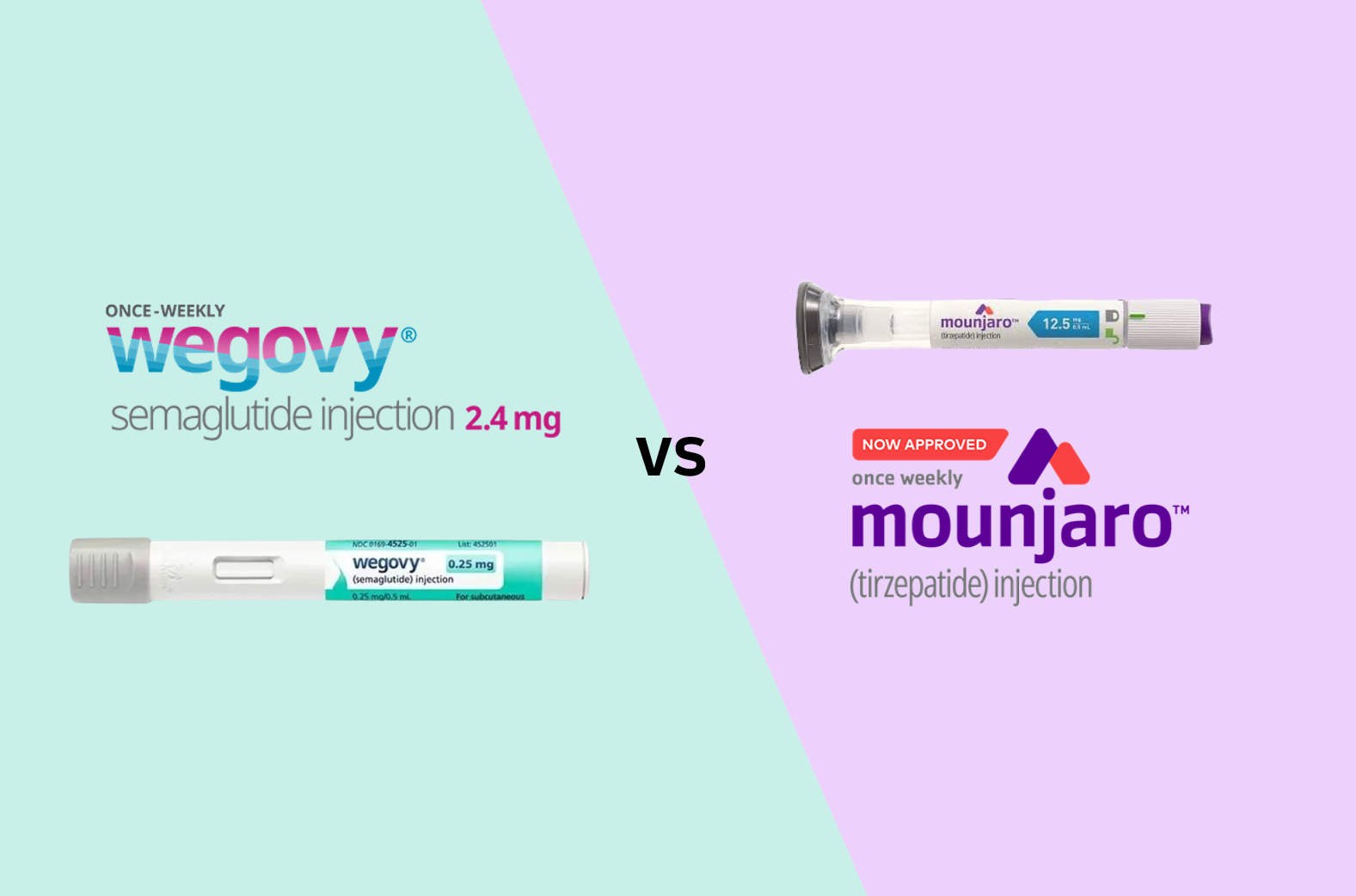
- "List of competing companies for obesity mkt half-finished"
- by Kim, Jin-Gu Sep 22, 2025 06:10am
- Following Novo Nordisk's signing of a co-promotion agreement with Chong Kun Dang for the obesity treatment 'Wegovy (semaglutide),' attention in the pharmaceutical industry has turned to which company will partner with Eli Lilly for the co-promotion of its rival product, 'Mounjaro (tirzepatide).' The pharmaceutical industry anticipate that Mounjaro's potential co-promotion partner will emerge after the Chuseok holiday. Once the partner is finalized, the competitive landscape for obesity treatments will be complete: Novo Nordisk·Chong Kun Dang versus the Lilly·Korean partner. According to industry sources on September 2, Eli Lilly Korea is officially maintaining its stance of selling Mounjaro alone. An official from the company said, "We are selling Mounjaro directly and distributing it through our directly contracted wholesalers," adding that "no decision has been made regarding a co-promotion with a domestic pharmaceutical company." However, it is reported that the company is discussing behind-the-scenes for a co-promotion partnership with domestic pharmaceutical companies. Last month, Lilly received interest from about 10 companies and is reportedly planning to select its final candidates after an internal review. An official from one of the companies that expressed interest told DailyPharm, "Eli Lilly Korea has scheduled to receive presentations from potential partners for Mounjaro after the Chuseok holiday," and added, "The competition among domestic pharmaceutical companies to secure Mounjaro is intense." Another industry official explained, "We submitted our proposal to Eli Lilly Korea last month, and Lilly is currently conducting an internal review. It was initially expected that the final candidate would be selected by the end of this month, but the timeline was pushed back to after the Chuseok holiday due to the lengthy internal review process." The potential co-promotion partners for Mounjaro are said to be three or four major domestic pharmaceutical companies with nationwide sales networks in Korea. These companies typically have a diverse portfolio of diabetes treatments, and some also have products in the aesthetics and plastic surgery sectors. Since Eli Lilly Korea is pursuing reimbursement for Mounjaro's diabetes treatment indication, discussions for a co-promotion partnership are reportedly centered on this specific indication. Once Mounjaro's co-promotion partner is decided after the Chuseok holiday, competition in the obesity treatment market is expected to intensify. On the other side, Chong Kun Dang and Novo Nordisk have already partnered, having signed an agreement on September 18 to jointly sell the obesity treatment Wegovy. The two companies will begin jointly handling sales and marketing for Wegovy in hospitals and clinics across the country starting next month. With the Chong Kun Dang·Novo Nordisk beginning to challenge the market with Wegovy, an intense competition against the Lilly·domestic partner is anticipated. While the initial battle will be for market leadership in the obesity treatment sector, the competition is highly likely to expand into the diabetes treatment sector in the future. Eli Lilly Korea is pursuing reimbursement for Mounjaro's diabetes indication with a goal of the first half of next year, and Novo Nordisk Korea is also conducting a reimbursement review for Ozempic, with the same-ingredient. An industry official predicted, "When Mounjaro's co-promotion partner is decided, the competitive landscape for the obesity treatment market will be completed," and concluded, "Future market share will largely depend on which patient groups domestic major pharmaceutical companies prioritize and how they secure a competitive advantage."
- Company
- CKD expands partnerships after concluding K-CAB deal
- by Kim, Jin-Gu Sep 19, 2025 06:14am
- Chong Kun Dang (CKD) has added the obesity drug Wegovy to its portfolio. This marks the company’s 10th sales and distribution agreement since ending its co-promotion deal for K-CAB (tegoprazan) with HK inno.N. Industry observers note that this move not only helps CKD minimize the void left by K-CAB but also diversifies the risks associated with co-promotion deals. On September 18, CKD signed a co-promotion agreement with Novo Nordisk Korea for Wegovy. Starting next month, both companies will jointly handle sales and marketing of the drug at domestic hospitals and clinics. According to IQVIA, Wegovy recorded KRW 213.3 billion in sales in the first half of this year. Analysts say CKD’s move to secure such a blockbuster product as a co-promotion item will help offset the loss incurred with the end of its K-CAB deal and stabilize future revenue growth. The company could also expect stable sales growth with the signing of the deal. Its total sales in 2023 stood at KRW 1.5846 trillion, down 5% from the previous year. The exit of K-CAB contributed to this decline. CKD has been co-promoting K-CAB with HK inno.N since 2019. The contract ended at the end of 2023, and HK inno.N has since partnered with Boryung for the co-promotion of K-CAB. CKD recognized KRW 137.6 billion in sales from K-CAB in 2023. This meant that 8% of its KRW 1.6496 trillion sales in 2023 had departed with K-CAB. In this situation, by securing the blockbuster item Wegovy, CKD has been able to minimize the K-CAB gap while ensuring stable sales growth. It also draws attention that this is the 10th sales and distribution agreement CKD has signed since the exit of K-CAB. Since the end of 2023, CKD has focused on signing joint sales and distribution agreements with domestic and global pharmaceutical companies. In January 2024, immediately after the termination of the co-promotion deal for K-CAB, CKD signed a co-promotion agreement with Celltrion Pharm for the liver agent Godex and the antihypertensive Dilatrend Tab. Then in February, it entered into a joint sales and distribution agreement with Bayer Korea for the chronic kidney disease treatment Kerendia Tab. In April, it agreed with SFI Health to exclusively sell and distribute the OTC brain function improvement drug Braining Cab. In May, CKD partnered with Daewoong Pharmaceutical for joint sales and distribution of Fexuclu Tab. Fexuclu is a P-CAB class treatment for gastroesophageal reflux disease, the same class as K-CAB, meaning CKD would compete with the very product it had just stopped selling. In June, CKD signed a distribution deal with Bayer Korea for Aspirin Protect and Adalat Oros. In November, it signed a joint sales and exclusive distribution agreement with GC Biopharma for the second-generation neutropenia treatment Neulapeg. In December, it entered a joint sales and distribution agreement with Alvogen Korea for the anemia treatment Nesbell. This year, the company continued to focus on expanding co-promotion partnerships. In February, it signed an exclusive sales and distribution agreement with Bayer Korea for the liver cancer treatments Nexavar and Stivarga. In March, it entered into a joint sales and distribution agreement with Pfizer Korea for the new pneumococcal vaccine ‘Prevenar 20’. Industry observers note that by diversifying its partnerships, CKD has been able to spread the risk associated with the termination of co-promotion agreements. This means that even if a situation like the termination of the K-CAB co-promotion agreement occurs in the future, the company can avoid a large-scale sales gap. Furthermore, with the addition of Wegovy, synergistic effects with CKD’s diabetes treatment portfolio are also anticipated. CKD possesses various diabetes treatments across multiple classes: DPP-4 inhibitors (Januvia, Janumet, Janumet XR), TZDs (Duvie, DuvieMet, Duvie-S), SGLT-2 inhibitors (Exiglu, Exiglu-M, Exiglu-S), and SUs (Neomaryl, Neomaryl-M). CKD acquired the domestic rights to the Januvia series from MSD in 2023. Duvie was developed by CKD itself. Wegovy contains the same active ingredient as Ozempic, which was approved as a diabetes treatment in 2022. Although it is approved as an obesity treatment, in addition to weight reduction, it also has blood sugar control effects. CKD is expected to promote Wegovy with its existing diabetes portfolio to target both obesity and diabetes patient groups, thereby expanding its influence in the endocrinology field. Analysts also note the possibility that the agreement could be expanded to include Ozempic. Ozempic is currently under reimbursement review by the government.
- Company
- AI usage-profitability disconnect…"perspective shift needed
- by Hwang, byoung woo Sep 19, 2025 06:13am
- Despite the increased use of Artificial Intelligence (AI) in the medical field, it is reportedly 'not profitable.' Some advised the need for new challenges to overcome systematic limitations. During the KHF2025 K-Digital Healthcare Summit on the 18th, Park Yong-min, a lead researcher at LG AI Research, suggested that for healthcare AI to be profitable, companies need to direct their business from hospitals to pharmaceutical companies and adopt new performance-based business models. Park Yong-min, a lead researcher at LG AI ResearchAccording to Park, three factors contribute to the reality that AI is 'not profitable' in healthcare: an oversaturated market, a structural limitation centered on on-premise systems, and AI's role as a supplemental tool detached from the core business. Park said, "The medical AI solution market has become so saturated, like a camera app market that anyone can easily jump into, that it's difficult to create a differentiated value." He pointed out that "With the rapid advancement and open-sourcing of AI technology in the last year or two, the difficulty of development has decreased, making it even harder to generate profits." Furthermore, Park explained that because hospitals, for safety reasons, insist on installing software on their own servers rather than in the cloud, the revenue for software companies is extremely low. For example, the software license accounts for only about 10% of the cost, while the remaining 90% covers ancillary expenses such as hardware installation and maintenance personnel, creating a structure where the software developer's share is minimal. Another barrier preventing the active use of this technology in the field is the lack of perceived intrinsic value in AI. While many medical AI companies sell their AI models, the argument is that because the products are treated as auxiliary tools separate from the core business, the value customers perceive is unclear. Park explained, "AI itself doesn't make money; the core business that embraces AI must be profitable." He added, "If medical AI is not linked to a hospital's core revenue, it becomes difficult for the decision-makers to justify spending money on it." 'Reimbursement and implementation delays' have been hurdles for medical AI…request prompted for a change in perspective Park also analyzed that structural obstacle in the industry are a significant factor in the lack of profitability for medical AI companies, citing a reimbursement system that does not translate technological advancements into increased revenue. "The system is structured so that AI created with technology from two years ago or the latest technology gets the same amount of money," Park stated. "Even innovative AI is facing difficulty in generating additional revenue." According to analysis by Park, the lack of incentives for technological advancement weakens companies' motivation to invest, resulting in a proliferation of similar technologies on the market. Park also pointed out that the process of adopting technology in hospitals is inefficient. To integrate an AI solution into a hospital's Electronic Health Record (EHR) system, it must undergo complex decision-making procedures, including review by each clinical department and the hospital's IT committee. "Assuming it takes about six months to adopt a specific solution, that's a long enough time for updated technology to emerge," Park said. "As a result, a technology gap can open up before both the medical professionals (the users) and the developers (the suppliers) can even feel the effects of the adoption." Related to this, the importance of shifting the business direction was emphasized. Park stated that AI's value would be recognized adequately if it were integrated into the value chain of pharmaceutical companies, which have larger budgets, rather than being limited to hospital services. For example, a health management app that collects a patient's daily data could be used as a tool to collect digital biomarkers for clinical trials or as a companion app for patient monitoring after a new drug is launched. Such usage would significantly increase its value and a pharmaceutical company's willingness to pay. "Even if it's the same technology, changing perspective from the current field to new drug development would open up a wider world," Park urged for a shift. Concluding his presentation, Park emphasized, "Medical AI must find a path to profitability." He pointed out that medical AI companies can only build sustainable businesses by adopting realistic strategic adjustments and fostering inter-industry collaboration, while acknowledging structural limitations.
- Company
- CKD-Novo Nordisk to jointly sell obesity drug 'Wegovy'
- by Kim, Jin-Gu Sep 19, 2025 06:13am
- Young-Joo Kim, CEO of Chong Kun Dang (left), and Kasper Roseeuw Poulsen, CEO of Novo Nordisk Korea (right), are signing a co-promotion agreement for Wegovy on September 18 at Chong Kun Dang Chong Kun Dang announced on September 18 that it has signed a domestic co-promotion agreement with Novo Nordisk Korea for the obesity drug Wegovy (semaglutide) at its headquarters in Chungjeongno, Seoul. Through this agreement, the two companies will jointly handle sales and marketing for Wegovy in hospitals and clinics across South Korea starting October 1. Wegovy is an injectable developed by Novo Nordisk with the active ingredient semaglutide. It is an obesity medication that aids in weight loss and reduces cardiovascular risk by suppressing appetite and increasing feelings of satiety. Launched in Korea in October 2024, it ranked first in domestic ethical drug sales for the second quarter of this year, according to IQVIA, a pharmaceutical market research firm. Wegovy is the only GLP-1 single receptor agonist (GLP-1 RA) and the only biologic among GLP-1 formulations. Wegovy shares 94% homology with the GLP-1 hormone produced in the human body. In the global pivotal trials, STEP 1 and STEP 5, Wegovy showed an average weight loss of 17%, with more than 20% weight loss confirmed in one-third of the subjects. Consistent weight loss effects and a strong safety profile were also demonstrated in the STEP 6, 7, and 11 clinical trials, which included Asian participants, including those from Korea. Wegovy is also the first and only obesity drug with an indication for reducing the risk of major adverse cardiovascular events (MACE). It has proven its ability to not only provide sustained weight loss but also to reduce the risk of major cardiovascular events independently of weight loss. A sub-analysis of the large-scale SELECT Phase 3 clinical trial, a cardiovascular outcomes trial (CVOT) in obese patients, showed a significant 37% reduction in the risk of major cardiovascular events within three months of administration (HR 0.63, 95% CI: 0.41-0.95). Within six months of administration, the risk of death from cardiovascular disease was reduced by 50% (HR 0.50, 95% CI: 0.26–0.93). In the heart failure patient cohort, the risk of hospitalization, urgent care, and cardiovascular disease-related death was reduced by 59% (HR 0.41, 95% CI: 0.24–0.67). Young-Joo Kim, CEO of Chong Kun Dang, said, "We have great expectations as we become a partner for Wegovy, a groundbreaking alternative in the obesity treatment field." Kim added, "Building on Chong Kun Dang's accumulated expertise from leading the hypertension, hyperlipidemia, and diabetes markets, accompanying disease of obesity, and our successful co-promotion experience with multinational and domestic companies, we will actively expand the domestic obesity treatment market." Kasper Roseeuw Poulsen, CEO of Novo Nordisk Korea, stated, "Through our collaboration with Chong Kun Dang, the company with a strong presence in the chronic disease sector in Korea, we will raise awareness of Wegovy's clinical benefits and actively support medical professionals in Korea, thereby contributing to improving the treatment environment for patients suffering from obesity."
- Company
- Will 'Bylvay' be listed in the second half the year?
- by Eo, Yun-Ho Sep 18, 2025 06:04am
- Attention has been drawn to whether Bylvay, the first drug in the Concurrent Approval-Evaluation-Negotiation Pilot Program, will be approved for the reimbursement listing. Ipsen Korea is currently in negotiations with the National Health Insurance Service (NHIS) over the drug price for Bylvay (odevixibat), a treatment for pruritus in patients aged 3 months and older with Progressive Familial Intrahepatic Cholestasis (PFIC). Bylvay recently passed the Health Insurance Review & Assessment Service's (HIRA) Drug Reimbursement Evaluation Committee (DREC) in July after a second review. It had previously been sent back for re-deliberation at the DREC in April. The government initiated the first phase of the Concurrent Approval-Evaluation-Negotiation Pilot Program in October of last year, selecting two drugs as its initial targets: 'Qarziba (dinutuximab),' a treatment for pediatric rare diseases, and Bylvay. The Concurrent Approval-Evaluation-Negotiation Pilot Program is a system designed to support swift insurance listing by conducting the Ministry of Food and Drug Safety (MFDS) approval, HIRA reimbursement evaluation, and NHIS drug price negotiation in parallel. However, questions were raised about the program's effectiveness in expediting drug listings when Bylvay initially failed to pass the first reimbursement hurdle. The review for Qarziba, the other drug in the first phase of the program, was also briefly halted at the DREC. Now that Bylvay has entered the final stage of negotiation, it remains to be seen if the Concurrent Approval-Evaluation-Negotiation Pilot Program can live up to its name by Bylvay's successful reimbursement listing. Meanwhile, the efficacy of Bylvay was proven in the Phase 3 ASSERT study, which was conducted on pediatric and adolescent patients up to 17 years of age. The study results showed that Bylvay met its primary endpoint by significantly reducing pruritus compared to the placebo. It also significantly improved the key secondary endpoints, including the mean serum bile acid concentrations at weeks 20 and 24 compared to placebo. These effects of Bylvay were sustained for up to 24 weeks of treatment.
- Company
- Rewriting the Medical Field with AI: KHF 2025
- by Hwang, byoung woo Sep 18, 2025 06:03am
- “Artificial intelligence (AI) technology is no longer just being applied to clinical settings; it is reshaping daily life.” Korea’s largest healthcare exhibition, the Korea-Hospital and Health Tech Fair (KHF2025), kicked off on the 17th at COEX in Seoul for three days. KHF2025 held its opening ceremony on the 17th and commenced its three-day schedule. Experts and stakeholders at the venue remarked that the medical field has now moved beyond simply adopting AI technology to actively exploring how best to utilize it. Now in its 12th year, the event highlighted the use of AI in hospitals and digital innovation across the sector. A wide range of players—from startups to public institutions—showcased their approaches to applying AI in healthcare, drawing significant attention. Right at the exhibition entrance, medical imaging company DK Medical Solution drew visitors’ attention with its equipment and technology that adopts medical AI. The company partnered with Google for the past 3 years, integrating Google Workspace collaboration tools and generative AI technologies into clinical workflows. DK Medical Solution showcased technology it developed in partnership with Google For example, AI agents can take care of hospital documentation and repetitive administrative tasks. A DK Medical Solution representative explained, “Previous AI adoption sometimes led to what we call ‘AI fatigue,’ placing burdens on medical staff. We found the solution through Google. In fact, hospitals that have implemented this system responded with comments like, ‘It’s much better than expected, beyond what we imagined.’” New AI technologies showcased by NIPA in the Digital Health Special Pavilion The National IT Industry Promotion Agency (NIPA), under the Ministry of Science and ICT, also participated in this exhibition, showcasing its digital health industry support strategies. NIPA has been overseeing medical AI projects for over a decade and responded swiftly to new developments—for instance, just three months after the emergence of ChatGPT last year, it began planning new projects in the healthcare field. The digital healthcare special hall organized by NIPA was structured around three themes: ▲Large-scale AI ▲DTx (digital therapeutics) ▲Public healthcare. Specifically, projects were unveiled for specialized counseling LLM services to manage chronic conditions in children and adolescents and to provide mental health care for depression and suicide prevention, as well as the development of digital therapeutics for conditions such as bruxism and irritable bowel syndrome. NIPA highlighted the companies and technologies it is supporting at its Digital Healthcare Special Pavilion. In particular, the AI-powered emergency medical network “Smart Ambulance” drew attention for its role in narrowing regional healthcare disparities. According to Myung-sook Yoon, a team leader at NIPA, the Smart Ambulance project was developed from 2019 to 2021 and is now in operation as an AI emergency system linking 119 ambulances with hospitals in real time in parts of Gangwon, Jeonnam, and Chungcheong (including Gwangyang and Yeosu) provinces. When a patient’s condition is recorded by voice in the ambulance, it is transcribed into text in real time and sent to the emergency room. The system also automatically displays bed availability at nearby hospitals using GPS, helping to reduce the so-called “ER ambulance carousel” problem. Yoon emphasized that the paradigm of medical AI is shifting. “In the past, domestic medical AI support was concentrated on diagnostic areas such as CDSS (Clinical Decision Support Systems) and medical imaging interpretation. Now, the focus is shifting toward pre-care (disease prevention) and post-care (prognosis management). For technology to take root in practice, it is crucial to enhance flexibility and usability at the level of the end user.” NIPA plans to continue supporting digital health policies through regulatory sandboxes and assisting regional hospitals in their digital transformation. AI is no longer novel - “We must consider what to use and how to use it” Industry stakeholders generally expressed positive expectations regarding the integration of medical AI, as observed through this event. At the same time, challenges remain. Hospital representatives visiting the booths remarked, “There are so many AI solutions that we don’t know which ones to actually use.” For this reason, experts at the fair predicted that the role of solutions would increasingly shift from merely developing AI suitable for clinical medicine to helping determine which AI systems to use. An industry official commented, “In clinical settings, the most common question is which AI solution to use among so many. Ultimately, finding the most optimized service will become critical. The consulting sector will also continue to expand, evolving into more customized services.” Many companies participating in KHF2025 prominently featured AI technology in their promotional activities. For instance, cost-related issues such as insurance reimbursement remain significant hurdles to adopting AI in healthcare. Experts were in consensus that institutional support is essential to ensure that the benefits of AI technology permeate every corner of the healthcare field. The experts particularly emphasized pan-ministerial cooperation. The Ministry of Health and Welfare should establish reimbursement policies grounded in safety and efficacy, while the Ministry of Science and ICT supports initial adoption through pilot projects and infrastructure development—a two-track approach. If regulators adopt a more flexible mindset and actively incorporate feedback from medical practitioners, the medical AI integration efforts highlighted at KHF2025 may well take root soon in more hospitals, pharmacies, and other care settings in Korea.