- LOGIN
- MemberShip
- 2025-12-22 04:48:25
- Company
- Vadanem for renal anemia makes its 'third attempt at reimb'
- by Nho, Byung Chul Mar 18, 2025 05:57am
- Mitsubishi Tanabe Pharma Attention has been drawn to the oral renal anemia drug Vadanem as the company completed meeting procedural requirements and attempts again to obtain reimbursement listing. According to industry sources, Mitsubishi Tanabe Pharma recently submitted Vadanem's drug pricing application to the Health Insurance Review and Assessment Service (HIRA). After obtaining approval from the Ministry of Food and Drug Safety (MFDS) in March 2023, Vadanem is making a third attempt at insurance reimbursement. After Vadanem obtained FDA approval in March 2024, it was listed in Germany for its demonstrated safety and efficacy. In January, it also secured a prescription recommendation from the U.K health authority As a result, Vadanem secured all medical health technology evidence required by the Korean health authority's listing criteria. Therefore, it is anticipated to be accepted. Mitsubishi Tanabe Pharma suggests a weighted average price of the substitute as about KRW 1 million to 1.2 million. Because the suggested price is about KRW 300,000 to 500,000 lower than the conventional EPO injectables, it has been evaluated to contribute significantly to saving the National Health Insurance finance. The efficacy of the drug was demonstrated through comparative effects (non-inferior) to a control drug. The side effect of the drug was reported to be similar to conventional drugs. Thus, it is being regarded as a new treatment choice. Anemia is caused by decreased kidney function and EPO production capacity, followed by lowered hematopoiesis. Renal anemia is accompanied by oxygen depletion due to decreased red blood cells, and it is commonly accompanied by in tiredness, decreased appetite, insomnia, and depression. It reduces the quality of life and impacts the mortality rate of patients. There are over 700 million patients with chronic renal kidney disease worldwide, and 1 out of 7 patients experience anemic symptoms. According to the National Health Insurance Service (NHIS) data, the number of patients with chronic kidney disease in Korea increased 36.9%, from 206,061 patients in 2017 to 282,169 patients in 2021. The increase was particularly steep in patients in their 80s, up 82.8%. Dialysis patients are also on the rise exponentially. Listing of competitive and new drugs may be justified as the National Health Insurance finance spent on approximately 100,000 patients amounts to KRW 3 trillion. Considering that these drugs are priced 30% less than injectable formulations and have improved convenience of administration, with equivalent effectiveness, it would be a significant loss in national finance. Meanwhile, the EPO formulation, developed 30 years ago, is the only available treatment for renal anemia. Third generation injectables with extended intervals of administration have been launched recently. However, many patients do not respond to these treatments, experience changes in blood pressure, and have adverse reactions, such as nausea and vomiting. Thefore, there is a need for treatments with new mechanism. Vadanem is a hypoxia-inducible factor (HIF) prolyl hydroxylase (PH) enzyme (HIF-PH) inhibitor. It works by improving hemoglobin levels by activating 'erythropoietin (EPO)' and reducing 'hepcidin,' a hormone responsible for iron metabolism. The domestic market for renal anemia drugs has been dominated by erythropoiesis-stimulating agents (ESAs). Hypoxia-inducible factor prolyl hydroxylase enzyme (HIF-PH) inhibitors are demonstrating potential after AstraZeneca·JW Pharmaceuticals·Mitsubishi Tanabe Pharma obtained approval from the MFDS for Evrenzo Tab (roxadustat)·Enaroy Tab (Enarodustat)·Vadanem Tab (vadadustat) in 2021·2022·2023, respectively. During this process, AstraZeneca withdrew from the launching of Evrenzo Tab in South Korea due to substantially lower drug pricing than the prime cost. According to a document on pharmaceutical distribution performance, external sales of renal anemia drugs amount to KRW 100 billion. The overseas market for all types of HIF-PHI prescriptions is worth KRW 10 trillion.
- Company
- Alteogen signs 2 licenses out agreements with AZ subsidiary
- by Cha, Jihyun Mar 18, 2025 05:56am
- Alteogen has signed two licensing-out agreements with AstraZeneca’s subsidiaries. According to the Financial Supervisory Service on the 17th, Alteogen has signed 2 exclusive license agreements with MedImmune, a subsidiary of AstraZeneca's bio R&D, for its subcutaneous (SC) formulation modification platform 'ALT-B4' based on recombinant human hyaluronidase enzyme. The company signed agreements with the UK subsidiary of MedImmune and the US subsidiary of MedImmune, respectively. The non-refundable upfront payment with the UK entity was KRW 36.4 billion. The technology fee (milestone payments) for development and commercialization is KRW 1.547 trillion, with separate sales royalties upon successful commercialization. Alteogen will receive sales royalties equivalent to a certain percentage of the net sales generated after the first commercial sale of products using ALT-B4. The upfront payment for the contract signed with the US corporation is KRW 29.1 billion. The milestone payment is 843.8 billion won, with separate sales royalties. The total upfront payment for the two technology export contracts signed by Alteogen is KRW 65.5 billion. The total milestone payment for the 2 contracts is KRW 1.8985 trillion. Alteogen's ALT-B4 technology can change an intravenous (IV) formulation to a subcutaneous (SC) formulation by hydrolyzing hyaluronic acid under the skin. Unlike the IV formulation that patients have to receive for 4-5 hours in the hospital, the SC formulation allows patients to self-inject the treatments at home in 5 minutes. Since 2019, Alteogen has signed a series of technology transfer agreements with global pharmaceutical companies including Merck (MSD) in the United States, Intas Pharmaceuticals in India, and Sandoz in Switzerland. Alteogen has licensed out its ALT-B4 technology to the global pharmaceutical company GPC for USD 1.373 billion in 2019, MSD for USD 3.865 billion in 2020, Intas for USD 109 million in 2021, and Sandoz for USD 145 million in 2022. Among these, the contract with MSD was extended by 4 months in February last year, increasing the contract amount by USD 432 million to USD 4.317 billion. The contract with Sandoz, signed in 2022, was replaced by a contract to develop an SC formulation biosimilar through the joint development of a new hyaluronidase in July. The specific terms and conditions of the contract and development strategy were not disclosed.
- Opinion
- [Reporter’s View] Being a global clinical trial powerhouse
- by Kim, Jin-Gu Mar 18, 2025 05:56am
- Korea is a global clinical trial powerhouse. According to the Korea National Enterprise For Clinical Trials, Korea's share of global clinical trials was 4.04% as of 2023. It is in 4th place after the United States (22.02%), China (13.59%), and Spain (4.09%). By city, Seoul has been in first place since 2017. Korea’s outlook is also positive. Korea’s global clinical trial market share rank rose one step each year, from 6th in 2021 to 5th in 2022 and 4th in 2023. The share gap with Spain is only 0.05%, and if the current trend continues, Korea is expected to rise to become one of the Top 3 clinical trial countries in the world. However, there are some drawbacks. Although Korea has established itself as a clear clinical trial powerhouse in terms of quantity, there are indications that it is not so in terms of quality. The most straightforward example is the clinical trials related to antibody-drug conjugates (ADCs), which have recently emerged as a new trend in drug development. According to the Korea National Enterprise For Clinical Trials, as of May last year, more than 600 ADC-related clinical trials were registered on ClinicalTrials.gov worldwide, but there is not a single ADC clinical trial registered or being conducted in Korea. This cannot be simply attributed to Korea’s small population. This is because 27 ADC clinical trials are underway in Taiwan, which has a population of about half that of South Korea. It is time to improve the quality of Korea’s clinical trials. In particular, improving regulations related to clinical trials may be a way to improve the quality of clinical trials. From this perspective, it is encouraging that the first step has recently been taken in the development of “decentralized clinical trials (DCT)”. DCTs refer to de-hospitalized clinical trials that collect clinical data using wearable or mobile devices and deliver test drugs by mail, etc. Patients can participate in clinical trials without having to visit a medical institution in person. A representative success story of decentralized clinical trials is Moderna, which developed the COVID-19 vaccine. The industry has consistently called for the introduction of decentralized clinical trials. In response, the government has decided to launch a pilot project for decentralized clinical trials starting this year. The government plans to conduct 6 decentralized clinical trials during the pilot project period until 2027, and then institutionalize the system based on these trials. Korea’s high-quality infrastructure is considered the main reason why Korea has grown into a global clinical trial powerhouse. This includes excellent medical staff, hospital facilities, and the high level of education of clinical trial participants. This has enabled Korea to become a clinical trial powerhouse in terms of quantity. However, there is still much that needs to be done in terms of quality. Now is the time to improve the quality of clinical trials based on excellent infrastructure. Regulatory improvement is the surest way to improve the quality of clinical trials. This can foster an environment in which clinical trials of advanced drugs such as ADC can be conducted in Korea. Only when innovative new drugs can be developed in Korea will Korea be able to go beyond being a clinical trial powerhouse and become a pharmaceutical powerhouse.
- Company
- Can the myelofibrosis drug Ojjara pass CDDC review in KOR?
- by Eo, Yun-Ho Mar 18, 2025 05:56am
- Industry attention is rising on whether GSK’s new drug for myelofibrosis, Ojjara, will be able to make progress in its reimbursement journey and be listed in Korea. According to industry sources, GSK's myelofibrosis treatment Ojjara (momelotinib) will be presented for review to the Health Insurance Review and Assessment Service's Cancer Disease Deliberation Committee tomorrow (19th). Specifically, the indication being reviewed is its use as a ‘treatment for adults with anemia at intermediate or high risk of myelofibrosis.’ The drug is currently indicated for primary myelofibrosis, post-polycythemia vera myelofibrosis, or post-essential thrombocythemia myelofibrosis. GSK recently launched Ojjara as a non-reimbursed drug. It remains to be seen whether the application will lead to the introduction of a covered treatment option that will significantly improve anemia, which has remained an unmet need in the treatment of myelofibrosis in Korea. Ojjara has a unique triple-inhibition mechanism that blocks JAK1, JAK2, and ACVR1 (Activin A Receptor Type 1). In the treatment of myelofibrosis, inhibition of JAK1 and JAK2 can contribute to the improvement of systemic symptoms and reduction of splenomegaly in patients, while inhibition of ACVR1 can help alleviate anemia by inducing a reduction in hepcidin expression. Managing anemia is one of the unmet needs in the treatment of existing patients with myelofibrosis. Anemia, which increases the need for blood transfusions, causes more than just dizziness, and depending on the severity, it can lead to a serious condition that can be life-threatening. The Phase III SIMPLIFY-1 and MOMENTUM studies have shown that, regardless of prior treatment with JAK inhibitors, Ojjara can significantly improve the main symptoms of splenomegaly and transfusion dependence in the treatment of patients with myelofibrosis with anemia. In the SIMPLIFY-1 study, which confirmed the clinical efficacy and safety of Ojjara compared to that of JAK inhibitors in the first-line treatment of patients with myelofibrosis who had no prior experience with JAK inhibitors, Ojjara demonstrated non-inferiority to JAK inhibitors in the primary endpoint of spleen volume response at Week 24 of treatment. The proportion of transfusion independence in each patient group was 66.5% for the Ojjara arm and 49.3% for the ruxolitinib arm, indicating that Ojjara showed significantly less transfusion dependency. “While JAK inhibitors, which were used in the treatment of myelofibrosis, showed effects in alleviating splenomegaly and systemic symptoms, they worsened anemia or increased the need for blood transfusions, which left an unmet need,” said Seo-Yeon Ahn, Professor of Hematology & Oncology at Chonnam National University Hwasun Hospital, “Ojjara has confirmed its significant clinical value in managing anemia, which is closely related to the prognosis of patients with myelofibrosis, and we expect that its launch in Korea will contribute to improving the treatment outcomes and quality of life of more patients.”
- Company
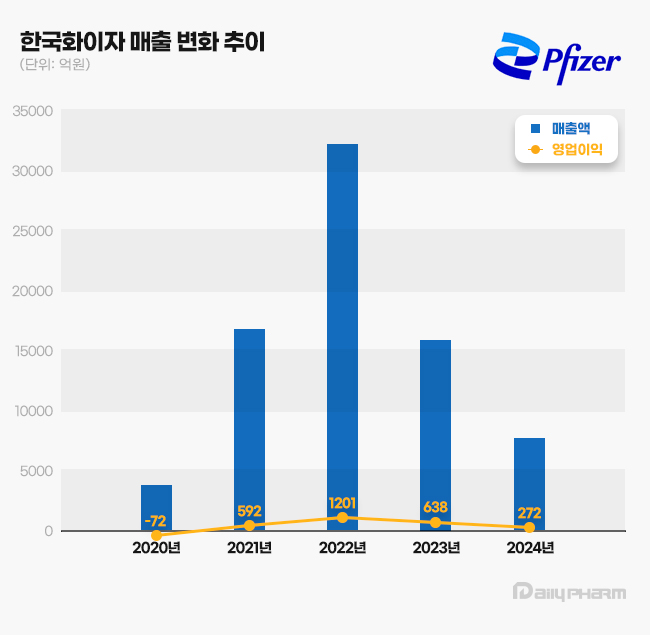
- Pfizer distributed KRW 160 billion dividend over 2 years
- by Chon, Seung-Hyun Mar 18, 2025 05:56am
- Pfizer Korea has decided on a large-scale dividend payout for the second consecutive year. While the company maintained an annual dividend policy of KRW 12.48 million, it has distributed KRW 160 billion to its parent company over the past two years. Large-scale profits during the COVID-19 pandemic enabled this high dividend. According to the Financial Supervisory Service (FSS) on the March 15, Pfizer Korea’s total dividend payout last year amounted to KRW 60.01 billion. It included an interim dividend of KRW 60 billion and an additional annual dividend of KRW 12.48 million. Pfizer Korea’s 2024 interim dividend was applied a 6,501% face value dividend rate, meaning shareholders received over 60 times the face value of KRW 5,000 per share. The interim dividend was distributed to 172,104 common shares, totaling KRW 55.9 billion, and 12,480 preferred shares, amounting to KRW 4.1 billion. Pfizer Korea made the second consecutive year of large-scale dividend payments after 2023. In 2023, the company distributed an interim dividend of KRW 100 billion and an annual dividend of KRW 12.48 million. The 2023 interim dividend was applied at a 10,835% face value dividend rate. Pfizer Korea The largest shareholder of Pfizer Korea is Pfizer’s subsidiary in the Netherlands, 'PF OFG South Korea 1 B.V.,' which holds a 99.99% stake in the company. Pfizer Korea significantly increased its dividend payouts as its sales surged during the COVID-19 pandemic. In 2020, Pfizer Korea recorded KRW 391.9 billion in sales. The sales more than quadrupled to KRW 1.694 trillion in 2021 and further skyrocketed to KRW 3.2254 trillion in 2022, an eightfold increase in sales over two years. Although its 2023 sales fell to KRW 1.6018 trillion, roughly half of the previous year's, it still was a fourfold increase compared to 2020. In 2020, Pfizer Korea reported an operating loss of KRW 7.2 billion and a net loss of KRW 21.2 billion. However, in 2022, its operating profit and net profit surged to KRW 120.1 billion and KRW 119.5 billion, respectively. In 2023, the company reported KRW 59.2 billion in operating profit and KRW 84.9 billion in net profit. Pfizer began its messenger RNA (mRNA) vaccine development in March 2020 in collaboration with BioNTech, using BioNTech's mRNA technology and Pfizer's extensive experience in global clinical trials. Within less than a year of COVID-19 spread, Pfizer successfully developed Comirnaty, a vaccine with 95% preventive effect. The U.S. Food and Drug Administration (FDA) granted it Emergency Use Authorization (EUA) in December 2020, and it received EUA approval in Korea in March 2021, leading to its full-scale supply through Pfizer's Korean subsidiary. Pfizer later developed the COVID-19 antiviral treatment Paxlovid. The Korean government used Paxlovid as a COVID-19 treatment. Pfizer Korea continued implementing a unique dividend policy, consistently paying KRW 12.48 million in annual dividends. The company calculates its dividend payout based on a 20% dividend rate applied to preferred share capital, which totals KRW 62.4 million. Pfizer Korea's total capital stands at KRW 922.92 million, with KRW 860.52 million in common shares (172,104 shares) and KRW 62.4 million in preferred shares (12,480 shares). Since 2005, Pfizer Korea has maintained a consistent dividend payout of KRW 12.48 million annually, based on a 20% preferred share dividend rate, except for four instances in the past 20 years. However, in 2017, the dividend payout was set at KRW 79.794 billion, exceeding net profit. At that time, the dividend rate was set at 660% of the face value (KRW 5,000 per share) for both common (2,455,520 shares) and preferred shares (12,480 shares), resulting in a significantly expanded payout. In 2008, the company allocated KRW 190 billion in dividends despite posting a KRW 600 million deficit that year, setting a 3045% dividend rate based on the face value. However, whether Pfizer Korea's high dividends will continue remains uncertain. In 2023, revenue fell 51.1% year-over-year to KRW 783.7 billion. Operating profit declined 57.4%, from KRW 63.8 billion to KRW 27.2 billion. The company's 2023 revenue and operating profit decreased 75.7% and 77.4%, respectively, compared to 2022, mainly due to the impact of entering endemic and declining COVID-19-related sales.
- Company
- Sanofi 'Dupixent' adds COPD indication
- by Whang, byung-woo Mar 17, 2025 06:00am
- 'Dupixent,' dominating the market for atopic dermatitis·asthma drugs, has expanded treatment areas to chronic obstructive pulmonary disease (COPD), thus gaining attention. Since Dupixent was approved for expanded reimbursement last year, the latest news on COPD indication will likely improve its prescription competitiveness. Product photo of DupixentAccording to pharmaceutical industry sources, Dupixent (dupilumab) was approved by the Ministry of Food and Drug Safety (MFDS) on the 13th for expanded indication to include add-on maintenance therapy to treat adult COPD who have an elevated blood eosinophil count and are not adequately controlled by standard inhaled therapy. Patients with COPD experience decreased quality of life due to trouble breathing, fatigue, and acute exacerbation, and the disease may lead to death if worsened. However, even if triple combination therapy, consisting of conventional inhalation therapy, is used, about 50% of patients still experience severe worsening. Therefore, patients have unmet needs for treatment. Dupixent works by targeting signaling pathway of interleukin (IL)-4 and IL-13, which are primary cause of type 2 inflammation. Dupixent became the first and only domestically approved targeted biologic medication for COPD. The drug is expected to provide new clinical benefits to patients with COPD who do not respond to conventional treatments. The current approval was based on two Phase 3 clinical studies, demonstrating a reduction in COPD annual rate of exacerbations and a significant improvement in lung function and patient quality of life. According to the Phase3 BOREAS and NOTUS, serving basis of expanded indication, at 52 weeks of Dupixent administration, the annual rates of moderate or severe exacerbations were 0.78 and 0.86, respectively, which were 30% and 34% lower than the 1.1 and 1.3 of the placebo group. The results met the primary endpoints for efficacy. Additionally, improvement in lung function started to show from week 2 of administration and maintained up to week 52. In the BOREAS and NOTUS clinical studies, the prebronchodilator FEV1 at week 12 increased from 77 mL and 57 mL of the placebo group to 160 mL and 139 mL with Dupixent, and FEV1 at week 52 increased from 70 mL and 54 mL to 153 mL and 115 mL, demonstrating significant improvement in effects. The St George's Respiratory Questionnaire (SGRQ) score of 4 or above had improved from 43% and 47% of the placebo group to 51.5% and 51.4% of the Duxient group. Both clinical studies showed a consistent safety profile of Dupixent, similar to previous studies. Kay Bae, Sanofi-Aventis Korea Country Lead, said, "COPD has a high disease burden due to acute exacerbations and lung function deterioration. However, it has high unmet needs because there are patients whose symptoms are not regulated with conventional treatments," adding, "The diagnosis rate is low. Thus, many patients who require treatment are not properly being treated." "As Dupixent is the first-and-only approved targeted biologic medication, it is expected to provide a new treatment paradigm for COPD. We hope that current approval will allow more patients with COPD to receive treatments, thereby improving their symptoms and quality of life," Bae said. According to Sanofi's reporting on performance, Dupixent's global sales for last year amounted to EUR 13.11 billion (approximately KRW 19.7 trillion), which was an increase of 23.1% from EUR 10.715 billion in 2023. The fourth quarter sales amounted to EUR 3.5 billion (approximately KRW 5.3 trillion), showing an increasing trend. In South Korea, Dupixent's sales surpassed KRW 100 billion, with KRW 105.2 billion in 2022, based on IQVIA. After that, it recorded KRW 143.2 billion in 2023, showing an increasing trend. Additionally, the impact of Dupixent is anticipated to grow due to the approval of expanded indication to include severe atopic dermatitis and drug switching between JAK inhibitors. Dupixient is effective in diseases that occur due to type 2 inflammation, including atopic dermatitis, asthma, chronic rhinosinusitis with nasal polyps, and eosinophilic esophagitis. It is expected to add indications in diseases with similar mechanisms. Sanofi is conducting Phase 3 clinical trials on Dupixent, aiming to secure indications in chronic spontaneous urticaria (CSU), chronic pruritus of unknown origin (CPUO), and bullous pemphigoid (BP).
- Company
- K-Bios busy developing new CAR-NK cell therapies
- by Son, Hyung Min Mar 17, 2025 06:00am
- The domestic pharmaceutical industry is initiating clinical trials for cell therapies and confirming new possibilities. GC Cell, Isu Abxis, Vaxcell Bio Therapeutics, GI Cell, and HK Inno.N are developing CAR-NK (chimeric antigen receptor) cell therapies. CAR-NK, which is derived from allogeneic cells, has the advantage of being able to compensate for side effects caused by the use of CAR-T cell therapies. CAR-T induces cytokines such as interleukin (IL) associated with neurotoxicity, but activated NK cells generally produce interferon-gamma (IFN-γ) and granulocyte/macrophage colony-stimulating factor (GM-CSF). As such, CAR-NK cell therapies are less likely to cause cytokine release syndrome (CRS) and neurotoxicity. CAR-T cell therapy is an immune cell therapy drug created by combining genetic information that expresses CAR into the patient's T cells. CAR-T has been proven effective in hematologic cancers and has been successfully commercialized, but its disadvantages include the lack of solid tumor indications, complex production process with CRS side effects, and high cost. GC Cell drives the development of CAR-NK cell therapy#EB According to industry sources on the 15th, GC Cell has recently started the first patient administration of GCC2005 (AB-205), a CAR-NK cell therapy candidate, in a Phase I trial. GCC2005 is a CAR-NK cell therapy that has improved the short duration of existing NK cells and enhanced efficacy by co-expressing CAR and IL-15. GC Cell has developed a method for culturing large quantities of highly active, high-purity NK cells from a small amount of cord blood. The Phase I trial aims to evaluate the safety and tolerability of GCC2005 in up to approximately 48 patients with relapsed/refractory NK and T-cell malignancies and to determine the maximum tolerated dose (MTD) and recommended Phase II dose (RP2D). Artiva Biotherapeutics Last November, GC Cell signed a third-party license agreement with its US affiliate, Artiva Biotherapeutics, and MSD to develop and commercialize two CAR-NK candidate substances, GC2005 and AB-201, using the affiliate’s intellectual property rights. The three companies terminated their joint research agreement in June last year, but will now work together again with this agreement. The candidate substances included in this contract utilize GC Cell’s CAR-NK platform technology and are new anticancer drug candidates that were previously developed through joint research between Artiva and MSD. According to GC Cell, the difference between this contract and the contract terminated in June is the main entity for research and development. CAR-NK development will be carried out by GC Cell, whereas Artiva was the main entity in the previous agreement. GC Cell has secured global exclusive rights to the CAR-NK candidate substances and will lead the research and development (R&D) in the future. In preclinical studies, GCC2005 showed anticancer effects in vivo in various CD5+ T-ALL models (RPMI-8402, CCRF-CEM). GCC2005 showed higher survival rates and tumor suppression efficacy compared to the control (vehicle). GC Cell is also developing the CAR-NK therapy AB-201. AB-201 targets solid tumors such as HER2-overexpressing breast cancer and gastric cancer. Artiva received approval from the US Food and Drug Administration (FDA) in 2022 for a Phase I/II clinical trial plan (IND) for AB-201. Since then, GC Cell has been conducting clinical trials after receiving approval for the Phase 1 IND for AB-201 from the Ministry of Food and Drug Safety and the Human Research Ethics Committee (HREC) of Australia in December last year. Through the trial, GC Cell plans to evaluate the safety and tolerability of AB-201 in patients with HER2-positive solid tumors and determine the recommended Phase II dose. Domestic companies also confirm the possibility of developing CAR-NK cell therapies Isu Abxis also recently released preclinical trial results and began full-scale development of CAR-NK cell therapies. The company's ISU104, which is under development, targets the HER3 (ErbB3) protein, which is mainly expressed in breast cancer. Isu Abxisand Seok-Ho Kim, a professor at Dong-A University's Department of Biomedical Engineering, has developed CAR-NK cells that have been engineered to express CAR cells targeting ErbB3 from cord blood-derived NK cells. The results of the research showed that when treating breast cancer cell lines with CAR-NK cells, the cancer cells were killed. Furthermore, in a mouse model implanted with breast cancer cells, ISU104-CAR-NK showed the effect of reducing the size of the tumor without any particular side effects. To date, no HER3-targeted anticancer drugs have been developed yet. Patritumab deruxtecan, an antibody-drug conjugate (ADC) that is in Phase II clinical trials by Daiichi Sankyo and MSD, is currently developed the furthest. Last year, Vaxcell Bio signed a business agreement with Bio Design Lab, a virus vector design company, to jointly develop CAR-NK cell therapies for the treatment of autoimmune diseases. Previously, Vaxcell Bio has signed MOUs with Bio Design Lab, Samsung Medical Center, and others to conduct research and development of new CAR-NK cell therapies. Under this agreement, Vaxcell Bio will provide third-generation NK cells and oversee the entire process of CAR-NK development, including research and clinical trials that meet GMP standards. Bio Design Lab will independently design and produce lentivirus vectors, one of the core technologies in CAR-NK cell therapy development. GI Innovation's affiliates GI Cell and Y Biologics signed a memorandum of understanding last year and began developing CAR-NK anticancer drugs. The two companies plan to develop anticancer drugs through GI Cell's CAR-NK cell therapy development and mass culture technology and Y Biologics' antibody discovery platform technology, Nanobody. GI Cell has completed a Phase I clinical trial in Korea for its NK cell therapy, T.O.P. NK, for patients with solid and hematological cancers. After proving the tolerability and safety of T.O.P. NK, GI Cell has been conducting a Phase IIa clinical trial since last month. GI Cell is embarking on joint research with HK Inno.N for a CAR-NK cell therapy. HK Inno.N and GI Cell are conducting basic research on 7 targets together. HK Inno.N is conducting two basic research projects on its own in addition to the joint research.
- Policy
- Five drugs all pass DREC's reimb review in February
- by Lee, Tak-Sun Mar 17, 2025 05:59am
- All five products, including new drugs and drugs that sought expanded indications, which were reviewed by the Health Insurance Review and Assessment Service's Drug Reimbursement Evaluation Committee in February, have passed review and will be negotiating the drug’s price with the National Health Insurance Service. Drugs that are subject to conditions of acceptance below the evaluated amount are also moving on to the negotiation process and are awaiting reimbursement. According to industry sources on the 14th, the National Health Insurance Service updated its negotiation subjects to include 5 drugs - Trodelvy Inj (sacituzumab govitecan-hziy), Cabometyx Tab (cabozantinib), Ebglyss Autoinjector Inj (lebrikizumab), Adempas Tab (riociguat), and Bimzelx Autoinjector Inj (bimekizumab). These five drugs are new drugs and drugs with expanded indications that were deliberated at the 2nd Drug Reimbursement Evaluation Committee meeting held on February 6. At the DREC meeting, Adempas Tab (for pulmonary arterial hypertension only) and Trodelvy Inj (for triple-negative breast cancer) were recognized as adequate for reimbursement. As such, drug pricing negotiations were expected. However, as new drugs such as Bimzelx (psoriasis) and Ebglyss (atopic dermatitis), and Cabometyx, which has applied for an expansion of its indication to clear cell renal cell carcinoma, will only be deemed adequate for reimbursement when the companies accept an amount below the evaluated amount, their negotiation results were expected to be unclear. This is because these companies must accept the evaluation amount set by DREC or below (less than the weighted average price of the alternative drug) for negotiations to proceed. For products that accept the results of the DREC deliberation, the Ministry of Health and Welfare will issue a negotiation order to proceed with negotiations with the NHIS on drug prices and expected claims amount. Accordingly, the 3 products that received conditional approval from DREC would have accepted DREC’s deliberation results to proceed with the pricing negotiations. In the case of Ebglyss, a drug for atopic dermatitis, it accepted a price below that of competing products such as Dupixent and Adtralza. Bimzelx, a psoriasis treatment, is also expected to cost less than Stelara or Cosentyx. The negotiation period is 60 days. Negotiations are expected to be completed before the Ministry of Health and Welfare's Health Insurance Policy Deliberation Committee (HIPDC) meeting in May, so it is expected that some of the drugs will be reimbursed as early as June 1. All three drugs, Tepmetko Tab and Vocabria Tab+ Vocabria Inj+ Rekambys inj, which passed DREC review in December last year and proceeded with drug price negotiations, have completed negotiations with the NHIS are likely to be reviewed by HIPDC this month.
- Company
- BESREMi lands in Big 5 Hospitals in Korea
- by Eo, Yun-Ho Mar 17, 2025 05:59am
- BESREMi, a new drug for polycythemia vera, has been approved for prescription at tertiary hospitals in Korea. According to the industry sources, PharmaEssentia Korea's BESREMi (ropeginterferon alfa-2b, a treatment for polycythemia vera, has recently passed the Drug Committees (DCs) of the Big 5 medical institutions in Korea, including Samsung Medical Center, Seoul National University Hospital, Seoul St. Mary's Hospital, Asan Medical Center, and Severance Hospital. As the drug’s reimbursement review is underway, the drug’s reimbursement listing is expected to quickly lead to actual prescriptions. Polycythemia vera is a rare blood disorder where a somatic cell mutation in the bone marrow abnormally activates bone marrow function and produces excessive red blood cells. It has a short survival period and is so fatal that 10~15% of patients with polycythemia vera develop myelofibrosis or leukemia within 10 years. Although hydroxyurea had been used as the standard of care, it was difficult to fundamentally cure the disease with hydroxyurea, and patients who could not be treated with hydroxyurea had limitations as there were practically no drugs available for them in Korea’s domestic reimbursement environment. BESREMi, an interferon treatment that selectively removes JAK2 mutations that cause polycythemia vera. In Korea, the drug received approval in October 2020 to treat low-risk and high-risk patients with polycythemia vera without symptomatic splenomegaly. The drug demonstrated its potential as a radical treatment for polycythemia vera in patients who had not received cytoreduction therapy or received less than 3 years of treatment with hydroxyurea. Therefore, whether the only interferon treatment option approved for polycythemia vera will be born in Korea is receiving attention. BESREMi demonstrated its efficacy and safety in the Phase III PROUD/CONTINUATION-PV trial that was conducted on polycythemia vera patients. Trial results showed that 53% of the patients in the Besremi arm achieved a complete hematological response, an improvement compared with the hydroxyurea patient arm (38%). The hematologic and molecular response rates at 72 months were also high, at 80.4% and 65.3% in low-risk and high-risk patients, respectively. Regardless of their risk, patients treated with Besremi did not require phlebotomy even 6 years after administration. Besremi is recommended as a first-line or second-line treatment for polycythemia vera in the National Comprehensive Cancer Network (NCCN) and European Leukemia Network (ELN) guidelines, regardless of previous treatment experience.
- Company
- Radioligand 'Pluvicto' available at tertiary gen hospitals
- by Eo, Yun-Ho Mar 17, 2025 05:59am
- Product photo of Pluvicto 'Pluvicto,' a new drug for prostate cancer, is now available for prescription at tertiary general hospitals. According to industry sources, Novartis Korea's targeted radioligand therapy, Pluvicto (Lutetium vipivotide tetraxetan), has passed the drug committees (DC) of the 'Big 5' hospitals, including Samsung Medical Center, Asan Medical Center in Seoul, Seoul St. Mary's Hospital, and Sinchon Severance Hospital, as well as the 17 medical institutes nationwide. A radioligand combines a therapeutic radioactive isotope with a ligand (targeted substance). A therapeutic radioactive isotope is released when radioligand binds to a targeted cell. This mechanism suppresses the proliferation of cancer cells. The MFDS designated Pluvicto, a treatment for metastatic castration-resistant prostate cancer (mCRPC), as the 6th medicine to be added to the 'Global Innovative products on Fast Track (GIFT)' following acknowledgment of the drug's innovativeness in June 2023. It was officially approved in May of last year. However, Pluvicto is still a non-reimbursed drug. Novartis is now preparing to apply for an insurance reimbursement listing. Pluvicto is a radioligand used to treat patients with prostate-specific membrane antigen (PSMA)-positive mCRPC who have been treated with androgen receptor (AR) pathway inhibition and 'taxane'-based chemotherapy. Pluvicto has been regarded as the next-generation innovative therapy that delivers a therapeutic radioisotope to prostate cancer cells by binding the radioisotope 177Lu to PSMA, ultimately killing cancer cells. Pluvicto was designated as an innovative drug and priority review drug by the U.S. Food and Drug Administration (FDA) and obtained FDA approval (March 2022). It was acknowledged for its innovativeness overseas. Meanwhile, the efficacy of Pluvicto was demonstrated through the Phase 3 VISION study. The combination therapy containing Pluvicto and the optimal standard therapy in study participants who have been previously treated with androgen receptor (AR) pathway inhibition and 'taxane'-based chemotherapy reduced mortality risk by 38% compared to the standard therapy alone. It has also statistically reduced the radiographic disease progression or death by 60%. Furthermore, approximately 1/3 (30%) of patients in the combination therapy group, treated with Pluvicto+standard therapy, who can be evaluated showed an objective response, compared to 2% of the monotherapy group.