- LOGIN
- MemberShip
- 2025-12-22 04:48:25
- Company
- Vyndamax is reimbursed for ATTR-CM in Korea
- by Whang, byung-woo Mar 06, 2025 05:58am
- Pic of Vyndamax Pfizer Korea announced on the 5th that its Vyndamax (tafamidis), a treatment for wild-type or hereditary transthyretin amyloidosis cardiomyopathy (ATTR-CM), has been granted reimbursement by Korea’s National Health Insurance. ATTR-CM is a progressive rare disease in which the naturally circulating transport protein in the blood, transthyretin (TTR), becomes unstable and separates into misfolded monomers, which accumulate in the heart and cause restrictive cardiomyopathy. According to this announcement, Vyndamax may be prescribed with reimbursement in adult patients aged 18 or older who have been diagnosed with hereditary ATTR-CM. Also, wild-type patients who satisfy all of the following conditions may receive the drug with reimbursement: those who ▲are Class I-III in the New York Heart Association (NYHA) heart failure severity classification for the last six months, ▲have received a diagnosis of heart failure and a history of one or more hospitalizations due to heart failure within the last six months, ▲has 600 pg/mL or higher level of pro-B-type natriuretic peptide (NT-proBNP, N-terminal pro-B-type natriuretic peptide level), and ▲have a left ventricular wall thickness at the end of diastole that is 12 mm or more. Vyndamax, which is the first and only approved treatment for adult patients with ATTR-CM in Korea, has secured clinical evidence through the ATTR-ACT study and the ATTR-ACT LTE study. In the ATTR-ACT study, which was conducted to compare the efficacy and safety of Vyndamax and placebo in 441 ATTR-CM patients, about 71% of patients in the tafamidis meglumine group were alive at the 30-month follow-up, showing improved survival compared to the placebo group (about 57%). It also reduced the relative risk of heart-related hospitalizations (0.48/year) by 32% compared to placebo (0.70/year) (95% confidence interval, 0.56-0.81). In addition, according to the results of the ATTR-CM LTE trial, which analyzed long-term survival rates of patients, the patient group that continued to receive tafamidis meglumine showed a reduction in all-cause mortality compared to the patient group that switched from placebo to tafamidis meglumine. Ji-Eun Lee, Head of the Specialty Care Business Unit at Pfizer Korea, said, ” We are pleased to be able to improve the access to treatment for our ATTR-CM patients who have had difficulty using the treatment due to financial constraints despite the availability of this option rather than heart and liver transplantation. We will continue to work to provide innovative treatments to patients with rare diseases, including ATTR-CM, and improve the treatment environment.”
- Company
- Novo Nordisk Korea appoints Kasper Roseeuw Poulsen as new GM
- by Whang, byung-woo Mar 06, 2025 05:58am
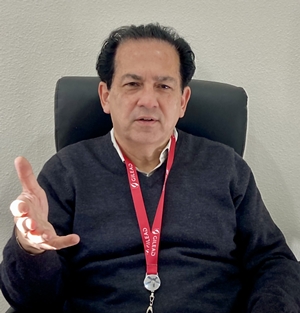
- Kasper Roseeuw Poulsen, Novo Nordisk Korea On March 5, Novo Nordisk Korea announced the appointment of Kasper Roseeuw Poulsen as the new General Manager starting March 2025. The new GM Kasper Roseeuw Poulsen joined Novo Nordisk in 2006 and served key roles in finance, strategy, organizational development, commercial partnership, and management across Europe, South America, and Asia-Pacific. Kasper Roseeuw Poulsen holds a bachelor's degree in Business Administration and a master's degree in Finance & International Business from Aarhus University's School of Business, Denmark. Until recently, he served as Vice President of Finance and Operations for Novo Nordisk's APAC region, overseeing more than 20 countries. Before that, he demonstrated outstanding strategy and executive ability as Vice President of a subsidiary in China. Kasper Roseeuw Poulsen said, "South Korea is a key market in the APAC region and a leading country for healthcare optimized for innovative medical settings. I'm excited to lead Novo Nordisk Korea." "By establishing closer partnerships with healthcare professionals and key healthcare partners in South Korea, we will strive to provide better benefits for patients based on Novo Nordisk's leadership in chronic diseases," he said. Meanwhile, the former GM Sasha Semienchuk was promoted to CVP Marketing in Novo Nordisk's subsidiary in China and will oversee commercial activities across the Chinese mainland. Since his appointment as Novo Nordisk Korea's GM in October 2022, Sasha Semienchuk had executed Novo Nordisk's patient-centered corporate value in the APAC region with his outstanding leadership. Sasha Semienchuk led the supply of products, such as Wegovy, for various treatment areas and fostered a corporate culture that embraces mutual growth between the company and its employees. He made significant contributions at Novo Nordisk, which earned international recognition as a 'Great Place to Work' and 'Best Workplace for Women' in two consecutive years.
- Company
- Pfizer launches JAK inhibitor for severe alopecia areata
- by Whang, byung-woo Mar 06, 2025 05:58am
- Pfizer Korea will launch a new Janus kinase (JAK) inhibitor treatment Litfulo (ritlecitinib tosilate), and set to challenge the market for severe alopecia areata. Previously launched Olumiant (baricitinib), the first drug approved in South Korea for treating adult patients with severe alopecia areata, has already settled in the market. The company will likely promote Litfulo's broader indication to treat adolescents over 12 years of age. Dr. Chong Hyun Won, Professor in the Department of Dermatology at Asan Medical Center in SeoulOn March 5, Pfizer Korea hosted a press conference celebrating the launch of the severe alopecia areata treatment Litfulo. The company highlighted the clinical significance of the drug. Litfulo is the first drug among alopecia areata treatments in South Korea to obtain approval for use in adolescent patients. Alopecia areata is an autoimmune disease that causes hair loss in the scalp, face, and body in patches or complete loss of hair. It is an inflammatory and immune-mediated disease caused by the immune system attacking the body's hair follicles, leading to hair loss. In South Korea, the number of patients treated for alopecia areata showed an increasing trend for the past 10 years, recording 154,380 patients in 2013 and 178,009 patients in 2023. In most cases, alopecia areata without severe symptoms naturally recover and respond well to treatments. However, it has a high relapse rate, with about 40-80% of patients experiencing relapse within a year. Dr. Chong Hyun Won, Professor in the Department of Dermatology at Asan Medical Center in Seoul, who attended the press conference, said, "About 100% of the patients with alopecia areata experience relapse within 20 years, so the disease has a high recurrence rate." Dr. Won explained, "It causes a substantial psychological burden on patients and is closely associated with mental health issues, such as depression, affecting the quality of life greatly." However, the introduction of JAK inhibitors like Litfulo has changed the treatment settings. Previously, severe alopecia areata was treated with corticosteroids or cyclosporine. Analysis suggests that aggressive treatment is possible after the introduction of a new option. "The launch of the new treatment provides hope for patients with unmet needs who suffered for a long time from alopecia areata. It is also meaningful to doctors, considering that a safe new option is now available," Dr. Won said. The basis of approval for Litfulo was the global clinical study Phase 2b/3 ALLEGRO. The analysis results evaluating the primary endpoint, the patient ratio with a Severity of Alopecia Tool (SALT) score of 20 or below, showed that at week 24, 23% of the patient group had a SALT score less than 20, which was statistically significant treatment effectiveness compared to a 2% in the placebo group. At week 48, the treatment group with a SALT score less than 20 was 43%, confirming significant treatment effectiveness than the placebo group (10%). This indicates that effectiveness increased over time. (from left) Dr. Chong Hyun Won, Professor in the Department of Dermatology at Asan Medical Center in Seoul, and SungBum Jung, Chief Medical Affairs at Pfizer When Olumiant was launched earlier, the alopecia areata had high unmet needs despite its non-reimbursed indication. It was evaluated that a higher-than-expected number of patients are opting for treatment. In other words, since Olumiant already dominates the market, the company must strategize to promote Litfulo. The most significant difference is the mechanism and indication. Unlike Olumiant, which targets JAK1 and 2, Litfulo primarily targets JAK3. Also, Olumiant is used for adults aged 18 and older, whereas Lifulo is used to treat adolescents aged 12 years and above. Dr. Won commented regarding this, "As of 2023, adolescents account for about 10% of the patients with alopecia areata, and the number can be lower with severity. However, the drug presents significance considering that earlier occurrence of alopecia areata may require longer treatment and has poor prognosis when relapse." Furthermore, Dr. Won mentioned that it is too early to determine drug switching between existing treatments and new treatments. "As drug switching requires the analysis of drug's effects and safety, a clear answer is not available at this point," he said. "We need confirmation of which patients can be better treated with existing treatment with longer safety."
- Policy
- CKD and Daewoong Bio enter donepezil-memantine combo market
- by Lee, Tak-Sun Mar 06, 2025 05:55am
- Chong Kun Dang Pharmaceutical and Daewoong Bio will enter the donepezil-memantine combination drug market that was launched this month. Although Chong Kun Dang and Daewoong Bio’s products were not included in the initial list of approved products, the companies will join the market in the form of a license transfer and co-promotion agreement. As both companies own the No. 1 and No. 2 products choline alfoscerate products in Korea -Chong Kun Dang Gliatirin and Gliatamin – which are brain function enhancers, their entry into the donepezil-memantine combination market is expected to increase the scale of product performance more than expected. According to industry sources on the 5th, Chong Kun Dang received permission from Korea Arlico Pharm to transfer the license for its donepezil-memantine combination drug and registered it with the Ministry of Food and Drug Safety in January. Chong Kun Dang Neuropezil M 10/20mg is the main product. The transfer of the license delayed the reimbursement listing process for the drug, which resulted in a later launch date than other pharmaceutical companies. This month, 7 donepezil-memantine combination drugs - Hyundai Pharm’s DM Duo Tab, Yungjin Pharm’s Demenduo Tab, Bukwang Pharm’s Ariplus Tab, Ildong Pharm’s Memansept Tab, Whanin Pharm’s Domentia Tab, Hutecs Korea Pharmaceutical’s Altsucomp Tab, Korean Drug’s Neurocept Duo Tab – were released to the market. Chong Kun Dang plans to release its product in April. Daewoong Bio will start selling Demenduo through a copromotion agreement with Yungjin Pharm starting this month. The donepezil-memantine combination was initially approved in the United States in 2014 and was then approved in Spain, Greece, and Croatia since, but this is the first time the combination was approved in Korea. The domestic patent holder is Hyundai Pharm, which has demonstrated equivalence and toxicity safety through comparative tests of donepezil and memantine administered alone and in combination. In Korea, it is used as an alternative to donepezil and memantine combination therapy for the treatment of moderate-to-severe Alzheimer's disease. The entry of Chong Kun Dang and Daewoong Bio in this dementia combination drug market is expected to heat sales promotion activities. The two companies have an established nationwide distribution network for geriatric drugs through their choline alfoscerate-based drugs. Last year, according to UBIST, Chong Kun Dang’s Gliatirin recorded KRW 121.3 billion in outpatient prescription sales, while Daewoong Bio’s Gliatamin recorded KRW 159.7 billion, continuing their popularity. However, choline alfoscerate’s reimbursement standard was reduced through a re-evaluation, and the Ministry of Food and Drug Safety is also conducting a clinical re-evaluation on its efficacy, so both companies had to look for products that can replace choline alfoscerate. Although the use of this dementia combination drug and the brain function enhancer choline alfoscerate are different, they are mostly used by the elderly, so it is analyzed that if the companies utilize their established distributor base, this may increase the companies’ short-term performance. Donepezil and memantine are the most widely used ingredients in the dementia drug market. Donepezil's original drug Aricept recorded KRW 95.8 billion in outpatient prescriptions last year, while memantine's original drug Ebixa recorded KRW 19 billion, with the combined prescription value of the two drugs exceeding KRW 100 billion. However, some analysts say that their expected market size is limited because the prescription rate of the combination of the two ingredients is smaller than that of each single ingredient. Interest is gathering as to whether the new dementia combination drug market, which has been joined by Chong Kun Dang and Daewoong Bio, which are strong players in the geriatric drug market, will see success in Korea.
- Company
- "COVID-19 response has changed to protect high risk groups"
- by Whang, byung-woo Mar 05, 2025 06:01am
- As COVID-19 transitioned to the endemic phase, an important issue has arisen regarding 'how' to prevent and respond to the disease, unlike the initial period focused only on response. One of the big changes was the reimbursement of treatments. On October 25, 2024, The Ministry of Health and Welfare (MOHW) approved the National Health Insurance reimbursement of the COVID-19 treatments, Veklury and Paxlovid. Based on the demands of clinical settings, the government aims to provide a stable supply of COVID-19 treatments to patients through the National Health Insurance system. In another point of view regarding infectious disease management in the endemic period, experts are highlighting the need to revisit the discussion of 'SARS-CoV-2,' which is one of the respiratory viruses other than COVID-19. Essy Mozaffari, Gilead Sciences Medical AffairsDuring the meeting with Daily Pharm, Essy Mozaffari, affiliated with the Gilead Sciences Medical Affairs, emphasized the role of antiviral therapy in protecting immune-compromised individuals and high-risk patients. In February 2020, the WHO officially announced the name for COVID-19, and at the same time, it assigned the name SARS-CoV-2 to the virus. It means that corona 19 (COVID-19) is typically used when discussing symptoms, whereas the SARS-CoV-2 virus causes the infection. Medical Affairs Mozaffari (hereafter, MA) said, "At the current endemic phase, it is crucial that we discuss SARS-CoV-2 infection rather than using the term COVID-19," adding that, "If SARS-CoV-2 is used to describe the virus, it will help remind that it is a virus that can make people ill every year." The latest COVID-19 responses have focused on immune-compromised individuals and high-risk patient groups, who can be relatively vulnerable to a disease. The approach has been limiting the spread of the disease through immunization and providing treatments to infected individuals in a timely manner. For instance, the COVID-19 treatment Veklury (remdesivir) is the first antiviral agent to receive approval from the U.S. FDA for the treatment of hospitalized adult patients with COVID-19. Veklury is now recommended as the standard therapy for adults and children who are hospitalized due to SARS-CoV-2 infection. Also, it is recommended for use in non-hospitalized patients with mild and moderate symptoms who are at risk of advancing to severe COVID-19. MA Mozaffari stated, "Although there are many antiviral therapies, Veklury has low drug interaction, so it is an important treatment option for patients who must take other medicines. Patients who have liver and spleen dysfunction can use the therapy without adjusting the dosage." "Veklury with real-world evidence demonstrated effects in high-risk patient group" MA Mozaffari particularly highlighted that Veklury has proven real-world evidence (RWE) in hospitalized patients due to COVID-19. "The Phase 3 PINETREE trial involving high-risk non-hospitalized patients infected with SARS-CoV-2 has shown that administering Veklury for three days decreased the hospitalization risk," MA Mozaffari said. "The recent real-world data (RWD) confirmed that the use of Veklury in the high-risk patient group, including immune-compromised individuals and older patients aged 65 and above, significantly lowered the death risk compared to the control group in all mutation periods. MA Mozaffari views that proper management of infection through treatments can benefit the efficient management of the medical healthcare system as medical healthcare system resources are being spent on managing immune-compromised individuals. "COVID-19 infection causes a significant burden to the medical healthcare system consistently, and it poses a risk of disease progression and death in older people aged 65 and above," MA Mozaffari said. "Antiviral therapies with proven treatment effects for various COVID-19 mutations will play a crucial role in future COVID-19 treatments." Now, Gilead Sciences is conducting research on the potential use of Veklury in a particular patient group with unmet needs for COVID-19 treatments. The company is evaluating the effects of Veklury treatment in new mutations as COVID-19 vaccines target changes. "Based on trial results so far, Veklury continued to maintain treatment effects on all mutations, including omicron sub-variants. Notably, there have been no key genetic changes affecting targeted RNA polymerase of the virus," MA Mozaffari explained. The results indicate that mutations to the virus will not cause significant changes to RNA structure and function, so the therapy can continue to work effectively," MA Mozaffari analyses. Lastly, MA Mozaffari mentioned the concern for effective responses amid COVID-19 settling down as an endemic disease. "COVID-19 is now transitioned to endemic disease, but SARS-CoV-2 continues to pose significant health risk worldwide," MA Mozaffari said. "The government, researchers, doctors, and individuals must strive to maintain the infection rate low and stay alert to respond to new mutations effectively."
- Policy
- Bill for vaccinating 'shingles for elderly·HPV for males'
- by Lee, Jeong-Hwan Mar 05, 2025 06:00am
- The Democratic Party of Korea Rep. issues a bill The Democratic Party of Korea is pursuing changes to the law to expand the free-of-charge vaccination program, requiring the government to cover the costs of shingles vaccines for adults 65 and above and human papillomavirus (HPV) vaccination for males below 17 years. Given that the Yoon Suk Yeol government's pledges during the candidacy to expand the National Immunization Program (NIP) to include shingles and HPV vaccines fell through, the National Assembly aims to implement this with the legislation to protect national health. On March 4, the Democratic Party of Korea Rep. Park Heeseong announced the bill to make partial revision to the 'Infectious Disease Control and Prevention Act.' Rep. Park Heeseong pointed out that the government made a candidacy pledge to provide shingles vaccinations for adults aged 65 and above and HPV vaccines for boys aged 12 and above. However, it was not included in the government budget, suggesting that the pledge has fallen through. Rep. Park Heeseong said that shingles vaccinations have high preventative effects, but since they are still non-reimbursed, this poses a substantial financial burden for individuals facing cost differences. Rep. Park Heeseong highlighted that HIP infection is part of the NIP, but the law limits the range of free-of-cost vaccination to females aged 12 or between 12 and 26. Rep. Park Heeseong believes that the government is not implementing vaccination despite proven evidence, including cost-effectiveness and disease burden, for introducing single vaccinations for older people free-of-cost and HPV vaccinations for males at no cost. Therefore, Rep. Park Heeseong drafted a bill to add shingles vaccination to the NIP and expand the HPV vaccination NIP to include males. The bill newly added·established Clause 18 to Article 24 of the NIP to include 'shingles.' The bill amended the current law to include a new 'Article 24-2 on human papillomavirus (HPV) infection vaccination.' The bill's amendment details that the mayor of a special self-governing city, governor of a special self-governing province, or the mayor·governor·head of Gu is now required to administer HPV vaccinations through local public health centers for females aged 26 or younger and males aged 17 or younger, as a measure to prevent HPV infection. Additionally, the bill's amendment to Article 64 (expenses paid by special self-governing provincess, cities, Gun, and Gu) now includes HPV vaccination. This change establishes the basis for local governments to cover vaccination costs, ensuring that patients can receive the vaccine free of charge.
- Opinion
- [Desk's View] Regulatory changes disrupt the generic mkt
- by Chun, Seung-Hyun Mar 05, 2025 06:00am
- The strategies of Korean pharmaceutical companies for entering generic markets have significantly changed over the past few years. Pharmaceutical companies made entries and withdrawals indiscriminately because of the government's regulatory changes. According to the Ministry of Food and Drug Safety (MFDS) report, prescriptions with approval declined by 35.6%, with 589 items. Compared to 4,195 counts in 2019, it shrunk by 86.0% over 4 years. The number of prescription drug approvals was 1,618 counts and 1,562 counts in 2017 and 2018, respectively. In 2019, it surged more than two-fold, with 4,195 counts. In 2020, it increased by 67.5% than two years before, with 2,616 counts. In 2021 and 2022, it decreased to 1,600 counts and 1,118 counts, respectively. In 2023 and last year, it was less than 1,000 counts. Although it may seem that pharmaceutical companies' motivation for entering the prescription drug business has decreased, the reality is that government has created regulatory confusion. In 2018, there was a ban on the sale of 175 pharmaceutical products containing the active ingredient valsartan, used to treat high blood pressure, due to excessive impurities. In response, the Ministry of Health and Welfare (MOHW) and the MFDS established the "Committee for Improving of Generic Drugs Policies" to formulate measures to control the excessive production of generics. The revised drug pricing system, implemented in July 2020, is one of the major policies by the government to suppress the overabundance of generic drugs. The revised drug pricing system requires generic products to meet both bioequivalence testing and the use of registered raw materials to maintain a maximum reimbursement price of 53.55% compared to the current patent-expired original drugs. The revised drug pricing system includes a stepwise pricing system, which involves a lower maximum reimbursement price for drugs that are newly listed for reimbursement. Pharmaceutical companies attempted to secure as many generics as possible before the government strengthened its regulations on generic drugs. It has been reported that most generics eligible for approval had already been obtained before implementing the new drug pricing system. However, many indiscriminately introduced generics failed to sell and eventually vanished from the market. In November last year, 1,000 drug items were removed from the National Health reimbursement list due to a lack of production or claims. Health authorities have recently been deleting drugs from the reimbursement list if there have been no insurance claim records in the past two years or if there has been no production or import data for three years. Among these 1,000 removed items, those approved in 2000 and 2019 were the most prevalent, accounting for 334 and 187 items, respectively. In other words, over half of the deleted drugs were new products on the market for less than five years. On May 1, 2023, 322 drug items were removed from the reimbursement list, with those approved in 2019 and 2020 were 221 items, which accounted for 68.6% of the total. The government’s regulatory strengthening encouraged pharmaceutical companies to obtain generic approvals indiscriminately, accelerating market saturation. Ultimately, many of these generics failed to sell, disappearing from the market while only losing unnecessary approval costs. Since 2021, the number of prescription drugs withdrawn from the market has exceeded the number of new approvals. Between 2015 and 2020, the annual approvals of new prescription drugs consistently outnumbered the products withdrawn. In 2015, there were 2,406 newly approved prescription drugs, more than twice the 977 canceled or withdrawn products. In 2016, new approvals were more than three times the number of withdrawals. In 2019, however, canceled or withdrawn products reached 1,283, amounting to only 30.6% of new approvals, and in 2020, new approvals exceeded market withdrawals by 691 products. In 2021, the number of canceled or withdrawn prescription drugs increased to 1,687, surpassing the 1,600 new approvals, and this gap gradually expanded. Last year, market withdrawals increased to 2,432, more than four times the 589 newly approved products. Analysis suggests that pharmaceutical companies indiscriminately secured generics in response to the government’s regulatory strengthening without thinking of countermeasures, disappearing in mass quantity from the market after a certain period, ultimately leading to significant social and economic cost waste. Additionally, critics point out that the government’s frequent regulation changes have exacerbated the abundance of generics and caused strategic confusion among pharmaceutical companies. In 2012, the MOHW abolished the stepwise drug pricing system through a revision. After that, it allowed pharmaceutical companies to actively launch generics, even in markets long past patent expiration, on the premise that they could still receive high prices despite a late market entry. However, due to the ongoing issue of the abundance of generics, the stepwise pricing system was reinstated after 8 years. Moreover, the mandatory production requirements for contract-manufactured generics have been repeatedly reversed. In 2014, the MFDS introduced the 'GMP Compliance Certificate' system, which exempted contract-manufactured generics from the requirement to submit GMP evaluation data for approval purposes. Then, starting in October 2022, the requirement for submitting GMP evaluation data for contract-manufactured generics was reinstated to strengthen quality and safety management. Yet, in October of last year, the requirement for GMP evaluation data covering the manufacturing process for outsourced drugs was waived again under regulatory relaxation. In response to the government's regulatory changes, pharmaceutical companies strategized to maximize profits, further disrupting the market. The government is partially responsible for failing to anticipate the market impact of these regulatory changes. Implementing policies aimed solely at suppressing the overabundance of generics without understanding market dynamics has resulted in unnecessary social costs. Government policies do not always yield favorable market outcomes. We want to ask whether the government has considered reviewing the generic-related policies implemented over the past few years. Their efforts failed to identify any positive outcomes from these regulatory changes. It has been reported that the government is considering a new system to cut generic drug prices. The government reviews the proposal to lower domestic drug prices by comparing them with those in eight major countries (the United States·Japan·Germany, the United Kingdom·France·Switzerland·Italy·Canada). They plan to adjust domestic prices to match the adjusted average price derived from six countries after excluding the highest and lowest figures among the so-called A8 nations. The pharmaceutical industry has strongly opposed this. The rationale is it's reasonable to consider market entry timing when comparing generic drug prices internationally. However, whether the government will hear the industry's concerns remains uncertain. There is a growing fear that, once again, a one-sided policy will be imposed, ignoring the warnings from the pharmaceutical industry. To minimize the failure of the government's policy, the government should at least listen to the voices of the industry.
- Company
- Ocrevus is reimbursed for relapsing multiple sclerosis
- by Whang, byung-woo Mar 05, 2025 06:00am
- Pic of Ocrevus On March 4, Roche Korea announced that its multiple sclerosis treatment drug Ocrevus (ocrelizumab) will be reimbursed by Korea’s National Health Insurance from March 1. According to the new announcement, Ocrevus will be covered as a monotherapy for patients with relapsing multiple sclerosis, which includes ▲patients with relapsing-remitting multiple sclerosis (RRMS) who are ambulatory and have failed or had insufficient response to first-line treatment (e.g., interferon beta-1b) and ▲patients with secondary progressive multiple sclerosis (SPMS). As a result, Ocrevus will be reimbursed for the relapsing-remitting type as a second-line treatment and the secondary progressive type as a first-line treatment. Relapsing multiple sclerosis (RMS) includes both relapsing-remitting and secondary progressive multiple sclerosis. Relapsing-remitting multiple sclerosis (RRMS) is the most common type of multiple sclerosis. The reimbursement application of Ocrevus was based on a wealth of clinical evidence on its utility, including the results of large-scale global Phase III clinical trial OPERA I & II and the 10-year analysis of the open-label extension study in patients with relapsing multiple sclerosis. In the OPERA I & II studies, the Ocrevus group showed a 40% improvement in the risk of confirmed disability progression (CDP) compared to the control group over 12 weeks and maintained a consistent effect over 24 weeks. The annual recurrence rate (ARR) was reduced by nearly half compared to the control group, and the average number of brain lesions per MRI scan was also significantly improved, confirming clinical efficacy. The clinical efficacy of Ocrevus was maintained even after 10 years of dosing. A 10-year follow-up analysis conducted in the open-label extension study of OPERA I & II showed that the Ocrevus-treated group achieved a steady decline in ARR over 10 years, with the 10-year ARR (0.017) being equivalent to approximately 1 relapse in 60 years. In particular, in both clinical studies, patients who received early treatment with Ocrevus in the early stages of the clinical trial showed more effective disease progression control and lower risk of disability compared to patients who started treatment later. No new adverse reactions or unexpected side effects were observed in patients who received Ocrevus for 10 years, confirming an overall favorable safety profile. “Recently, treatment for multiple sclerosis has been shifting to a strong initial treatment strategy that actively prevents disability by using high-potency drugs from the early stages,” said Professor Ho-jin Kim of the Department of Neurology at the National Cancer Center. ”With the reimbursement of Ocrevus increasing the treatment options, more patients can effectively prevent disease progression and disability from the early stages, ultimately improving treatment outcomes.” “Ocrevus, which has risen to record number one in global drug sales at Roche, is a representative multiple sclerosis treatment that has benefited more than 350,000 patients worldwide,” said Ezat Azem, General Manager of Roche Korea. “We expect that the reimbursement application will strengthen the accessibility of treatment for patients with relapsing multiple sclerosis in Korea and provide more patients with the therapeutic benefits of Ocrevus, which have been confirmed through a large number of clinical data and prescription experiences.” Meanwhile, in Korea, Ocrevus was approved by the Ministry of Food and Drug Safety in May 2024 for two types of patients: relapsing multiple sclerosis (RMS) and primary progressive multiple sclerosis (PPMS).
- Company
- Pfizer’s sales fall 76% in 2 yrs with the end of pandemic
- by Son, Hyung Min Mar 05, 2025 06:00am
- Pfizer Korea’s sales are on a downward trend. The company's sales have plummeted by 76% in 2 years. The analysis is that the demand for COVID-19 vaccines and treatments has fallen sharply, which has affected the decline in sales. Pfizer Korea aims to make a rebound in sales with new products such as Prevnar 20, a new pneumococcal vaccine, and a COVID-19 vaccine that can respond to new variants. According to the Financial Supervisory Service on the 4th, sales of Pfizer Korea fell 51% from KRW 1.6018 trillion in 2023 to KRW 783.7 billion last year. Operating profit fell 57% from KRW 63.8 billion to KRW 27.2 billion over the same period. This is the first time in 4 years since 2020 that Pfizer Korea has recorded sales of less than KRW 1 trillion. Prizer Korea suffered a direct hit to its sales in the endemic. The company entered the KRW 1 trillion club in sales in 2021 with its COVID-19 vaccine, Comirnaty Inj, and its COVID-19 treatment, Paxlovid, but its sales have dropped sharply with the stabilization of the COVID-19 pandemic. Pfizer Korea Pfizer joined forces with BioNTech in March 2020, when COVID-19 began to spread around the world, to develop a messenger ribonucleic acid (mRNA) vaccine. BioNTech, which owned the mRNA technology, and Pfizer, which has extensive experience in large-scale global clinical trials, have produced synergy. Pfizer succeeded in developing the vaccine Comirnaty, which has a 95% preventive effect, in less than a year after the spread of COVID-19. In December 2020, the US Food and Drug Administration (FDA) granted emergency use authorization, and emergency use authorization was granted in Korea as well in March of the following year, after which the vaccine was supplied through the Korean subsidiary in earnest. Afterward, Pfizer succeeded in developing the COVID-19 treatment Paxlovid, which the Korean government also procured to use as a treatment. As a result, sales at Pfizer Korea also increased significantly. The company's sales reached KRW 1.694 trillion in 2021, surpassing the KRW 1 trillion mark, and then rose sharply to KRW 3.2254 trillion in 2022. Compared to the sales in 2020, sales increased by 723% in 2 years. However, sales began to decline in 2023 as governments around the world declared an end to the COVID-19 pandemic. Sales of Pfizer Korea in 2023 fell 50% year-on-year to KRW 1.6018 trillion, and the company failed to secure sales of KRW 1 trillion last year, at KRW 783.7 billion. Last year's sales were down 76% from 2022 when the company made the highest performance ever. Operating profit was also struggling. After recording an operating loss of KRW 7.2 billion in 2020, the company succeeded in turning a profit in 2021 with KRW 59.2 billion. After that, its sales jumped to KRW 120.1 billion in 2022 but decreased 47% to KRW 63.8 billion in 2023. Last year, it decreased by 57% from the previous year to KRW 27.2 billion. Aims to boost sales with the new product launch PfizerPfizer Korea is aiming to boost sales with the launch of a new product. The company launched a new pneumococcal vaccine, ‘Prevnar 20,’ in November last year. Prevnar 20 is a new pneumococcal vaccine that Pfizer introduced 14 years after the release of Prevnar 13. This vaccine adds seven serotypes (8, 10A, 11A, 12F, 15B, 22F, and 33F) to the 13 serotypes in the existing Prevnar 13. In clinical trials, Prevnar 20 demonstrated immunogenicity and tolerability against 20 serotypes when administered to healthy infants four times. These results were similarly shown in clinical trials conducted on adults. Sales growth is also expected for the non-small cell lung cancer drug Lorviqua. Currently, Pfizer Korea is in negotiations with the National Health Insurance Service to expand the reimbursement coverage of Lorviqua as a first-line treatment. Lorviqua is Pfizer’s third-generation ALK-positive non-small cell lung cancer targeted therapy. Currently, Takeda's Alunbrig and Roche's Alecensa, along with Lorviqua, have been fiercely competing in the second-generation ALK-positive non-small cell lung cancer targeted therapy. It will be interesting to see if the company can stay ahead of the competition in the first-line treatment environment, as the company confirmed Lorviqua’s efficacy with the latest data from the 5-year trial. Pfizer also plans to launch new vaccines that can respond to new variants to defend its sales. Pfizer introduced Comirnaty JN.1, a COVID-19 vaccine that can respond to new variants, including JN.1 last year. The company is also aiming to rebound sales by recently launching Comirnaty JN.1 0.033, a COVID-19 vaccine for infants, to make a rebound in sales.
- Policy
- MFDS designates etomidate a psychoactive drug
- by Lee, Hye-Kyung Mar 04, 2025 05:57am
- The Ministry of Food and Drug Safety (Minister Yu-Kyoung Oh) announced on February 28 that it will preannounce an amendment to the Enforcement Decree of the Narcotics Control Act that will designate 7 substances, including hexahydrocannabinol, which is scheduled to be designated as a controlled substance by the United Nations, as narcotics or psychotropic substances. The amendment is open for opinion collection until April 10. Five substances (4 narcotics and 1 psychotropic drug) that will be newly designated as narcotics this time are those designated as narcotics or psychotropic drugs at the 68th United Nations Commission on Narcotic Drugs (CND) and two psychotropic drugs including etomidate that have been designated as narcotics by the Narcotics Safety and Risk Management Deliberative Committee. Substances newly designated as narcotics by the United Nations Commission on Narcotic Drugs are new narcotics synthesized by changing the structure of existing narcotics. The Ministry of Food and Drug Safety is quickly identifying international narcotics trends and has already designated and managed some drugs as temporary narcotics. The proposed revision also includes etomidate, a general anesthetic induction agent. Since there were cases of illegal administration or abuse of etomidate in some medical institutions, it will be designated as a narcotic drug in advance and actively managed for their safe use in Korea. The Ministry of Food and Drug Safety said, “We expect that this designation of narcotics will be in harmony with international drug regulations and will actively respond to the problem of domestic drug abuse. We will continue to do our best to safely manage narcotics for the health and safety of the people.”