- LOGIN
- MemberShip
- 2025-12-22 04:48:25
- Company
- Reimbursement possible for Long-acting HIV treatment in KOR
- by Whang, byung-woo Mar 04, 2025 05:57am
- Expectations are growing in the clinical field with the imminent reimbursement of the long-acting HIV (human immunodeficiency virus) treatment ‘Vocabria+Rekambys’ combination in Korea. It has been more than two years since the combination was approved in Korea, but it has not yet been released on the market due to hurdles including costs. As patients have been waiting for its release, it is expected to quickly gain influence with reimbursement coverage. Pic of VocabriaAccording to industry sources, GSK Korea concluded drug price negotiations with the National Health Insurance Service for the combination therapy of the new HIV drugs Vocabria (cabotegravir) and Rekambys (rilpivirine). Rekambys Janssen Korea’s product and GSK was in charge of its reimbursement listing process in Korea. Both drugs were originally developed as oral medications and then developed into injectable drugs. Long-acting injectable drugs cannot cure HIV infection, but they are therapeutic agents that target white blood cells to help lower and maintain the level of the AIDS virus. In February 2022, it was approved by the Ministry of Food and Drug Safety as a combination therapy for the treatment of HIV-1 infection in adult patients who are virologically suppressed, have no history of virological failure, and have no known or suspected resistance to cabotegravir or rilpivirine. Currently, the market is divided between the three-drug combination therapy, Biktarvy (bictegravir/emtricitabine/tenofovir alafenamide, B/F/TAF) and the two-drug combination therapy, Dovato (dolutegravir/lamivudine). Although many prescriptions have been made before Biktarvy and Dovato, like Gemvoya and Triumeq are still being prescribed, the weight has shifted to using the later released treatments. According to the pharmaceutical research institution IQVIA, Biktarvy’s sales in 2023 had been KRW 54.5 billion, the highest among HIV treatments. This is an 11% increase compared to the KRW 49.1 billion in sales in 2022. Dovato also has a growth curve of KRW 13.2 billion in 2021, KRW 20.3 billion in 2022, and KRW 26 billion in 2023, after generating KRW 1.8 billion in sales at the time of its reimbursement approval in 2020. The biggest strength of the Vocabria+Rekambys combination that has emerged in this situation is its convenience. While existing HIV treatments are oral drugs that must be taken every day for 365 days a year, the combination therapy that includes Vocabria can reduce the frequency of administration to a maximum of six times a year with intramuscular injections administered once a month or once every two months. This strength is regarded to be effective in alleviating the anxiety of social stigma, which is considered a challenge for people living with HIV. According to a survey conducted by Love for One, an organization for people living with HIV, 73% of people living with HIV in Korea said they were afraid that taking HIV medication would reveal their infection to others and the surrounding environment. As there are already inquiries from patients about the combination therapy Vocabria+Rekambys in the clinical setting, experts believe that there will be a lot of switching of treatments. “The existing treatment requires taking one pill every day, so people have to take it in the middle of work or face stressful situations such as business trips or travel,” said Jin-nam Kim, a professor of infectious diseases at Hanyang University Hospital. ”Even before its release, there were patients who inquired about the treatment because they could avoid having to think about their daily lives if they could just get a shot at the hospital once a month.” As the number of treatments that require periodic injections, such as rheumatism and atopic dermatitis, has increased, it is believed that this may reduce the burden of social stigma felt by patients. However, the combination therapy of Vocabria+Rekambys is not all-encompassing, so the influence of existing treatments is expected to remain. Conventional treatments are usually prescribed at a hospital visit every 3 months, and in some cases, every 6 months. However, since the combination therapy is an injectable, the patient must follow the dosing cycle, and if it is difficult to shorten this cycle according to individual circumstances, it may be a burden to visit the hospital more frequently. Professor Kim said, “Adherence to medication is important, and in the case of oral medications that are taken daily, if the patient has the existing medication, they can take it daily and maintain the drug concentration. However, although there is a seven-day margin before and after the administration date for injections, there are indeed limitations depending on the patient.” The combination therapy of the two drugs is expected to be reimbursed by the National Health Insurance soon after it is approved by the Health Insurance Policy Deliberation Committee. In response, Professor Kim said that he could not make a definite statement as no treatment has been released yet, but based on patient inquiries, he expected that at least 10% of patients would switch. He added, “Injectable drugs cause pain at the injection site, and there are new drugs, so I don't think many will change at once. Still, the number of patients who inquired was in the double digits (more than 10%), and since the efficacy has already been proven through various studies, some patients will switch when provided with more options.”
- Company
- Potential blockbuster drug Kerendia…1yr since reimbursement
- by Whang, byung-woo Mar 04, 2025 05:57am
- The prescription performance of Kerendia (finerenone), Bayer’s treatment for chronic kidney disease in adults with type 2 diabetes, has been increasing since it was granted reimbursement last year. With its monthly sales recording KRW 1 billion in the last month of last year, the drug is rapidly building up its performance, and given its growth, it is likely to become a blockbuster treatment in Korea this year. Pic of Kerendia Tab Kerendia is a first-in-class, selective, non-steroidal mineralocorticoid receptor antagonist(MRA) that inhibits the overactivation of mineralocorticoid receptors, which can cause inflammation and fibrosis in the kidneys, kidneys, and blood vessels. Kerendia, which was approved in Korea in May 2022, was approved for insurance reimbursement benefits on February 1 of last year, about a year and a half after its approval in Korea. The standards for Kerendia’s reimbursement are as follows: Adult patients with type 2 diabetes who have been taking angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) for more than four weeks, but have ▲a urinary albumin-to-creatinine ratio (uACR) over 300 mg/g or a urine dipstick test result of 1+ or higher, and ▲an estimated glomerular filtration rate (If eGFR is between 25 and 75, the drug may be administered together with ACE inhibitors and ARBs). Kerendia gained the spotlight as diabetes accounts for the highest proportion (38.6%) among the causes of end-stage renal disease. Until now, drugs to control blood pressure and reduce the burden on the kidneys were used with GLP-1 and SGLT-2 inhibitors to control blood sugar, but there was an unmet need. In particular, as there had been no drug that could directly suppress chronic inflammation or fibrosis of the kidneys, Kerendia, which has a new mechanism of action that can directly target these, is expected to play a greater role. “So far, GLP-1 receptor agonists, SGLT-2 inhibitors, and RAS inhibitors, which are blood pressure medications, have been used to treat patients with diabetes and kidney disease, but the risk of chronic kidney disease persisted in the patients,” said Yong-Ho Lee, Professor of endocrinology at Severance Hospital and Director of General Affairs of the Korean Diabetes Association. “As Kerendia has proven its efficacy in various clinical trials, it will become an important treatment option for patients with chronic kidney disease,” he said. Monthly Sales of Bayer In fact, Kerendia‘s sales have been growing since its reimbursement in Korea. After being granted reimbursement last year, Kerendia’s monthly sales started at KRW 30 million in March and continued to rise, reaching KRW 100 million in April. In particular, the company recorded monthly sales of KRW 1 billion in December, the last month of last year, and is expected to continue to increase its influence this year. Looking at the quarterly figures, the company showed twofold growth each quarter, posting KRW 800 million in the second quarter, KRW 1.7 billion in the third quarter, and KRW 2.7 billion in the fourth quarter. Taking this into account, sales are expected to easily exceed the KRW 10 billion mark which is the threshold for a blockbuster drug in Korea, within this year. The expansion of the prescription of Kerendia seems to have been influenced by its characteristics as a treatment for chronic kidney disease patients with Type 2 diabetes. According to UBIST, prescriptions increased significantly in the early days after the reimbursement was applied, mainly in the field of nephrology, but the number of prescriptions in the field of endocrinology also increased from September, and in December, when monthly sales reached KRW 1 billion, the number of prescriptions in the field of nephrology and endocrinology did not differ significantly. Quarterly Sales of Bayer In this situation, the drug’s influence in the market is expected to continue to grow as Bayer Korea announced plans to expand Kerendia’s indications. On November 20, 2019, the Ministry of Food and Drug Safety approved a randomized clinical trial to determine the efficacy and safety of finerenone on the morbidity and mortality of heart failure patients with a left ventricular ejection fraction of 40% or more who were hospitalized due to an acute non-reversible episode of heart failure. It can be regarded as a domestic version of the Phase III FINEARTS-HF trial, which evaluated Kerendia in patients with heart failure with a left ventricular ejection fraction of 40% or more, which was announced at the European Society of Cardiology's annual conference (ESC 2024) in September last year. As Kerendia has already been shown to prevent heart failure-related secondary events in patients with heart failure with reduced ejection fraction (HFmrEF) and heart failure with preserved ejection fraction (HFpEF), which have ejection fraction 40% or higher, the indication expansion in Korea is not expected to be difficult if there are no major variables.
- Company
- Commercialization of PAH drug 'Winrevair' imminent
- by Eo, Yun-Ho Mar 04, 2025 05:57am
- Product photo of Winrevair The new drug 'Winrevair' for pulmonary arterial hypertension (PAH) is anticipated to land in South Korea. According to industry sources, MSD Korea's Winrevair (sotatercept), the world's first inhibitor therapy to treat PAH, has passed the secondary evaluation for the approval-reimbursement linkage process and now enters the last phase of the review. Considering that a typical review time for drug candidates submitted to the 'Pilot Project for Integration of Product Approvals, Reimbursement Coverage Reviews, and Drug Price Negotiations' has shortened to 81.5 days, the approval for Winrevair will be made soon. Since the reimbursement review has also started, it is to be closely watched whether Winrevair will gain presence as a treatment option in South Korea. Winrevair was designated an orphan drug by the Ministry of Food and Drug Safety (MFDS) in January and designated as the Global Innovative products on Fast Track (GIFT) in April. Additionally, the U.S. Food and Drug Administration (FDA) officially approved Winrevair as a subcutaneous injection administered once every 3 weeks to treat PAH. Winrevair is designed to bind the protein complex activitin and transforming growth factor-β (TGF-β). This drug works by inbiting abnormal signaling bewteen pulmonary vascular endothelial cells and reversing the disease progression. PAH is caused by narrowing of pulmonary arteries, leading to an increase in pulmonary artery pressure, and ultimately resulting in cardiac failure. In South Korea, almost half of the patients with PAH die within 5 years. More than 10 drugs have been approved to treat PAH, including phosphodiesterase type 5 (PDE5) inhibitors and endothelin receptor antagonists. However, many patients suffer from serious symptoms despite undergoing 2-3 combination therapies. Meanwhile, the effectiveness of Winrevair compared to the placebo was confirmed in the Phase 3 study of Winrevair named STELLAR. The clinical study evaluated the effectiveness and safety of the drug, assigning patients to the Winrevair treatment group and the placebo group on 1:1 ratio. The clinical study results have shown that Winrevair extended 6 Minute Walk Distance (6MWD), the primary efficacy endpoint, by 40.1m. The placebo reduced the 6MWD by 1.4m. 38.9% of the patients treated with Winrevair had significantly improved multiple endpoints, including improvement in the secondary endpoint increase in 6MWD over 30m. This was about four-fold longer than 10% of the placebo group.
- Company
- Will COVID-19 vaccines be included in the NIP?
- by Moon, sung-ho Feb 28, 2025 05:58am
- The final results are gaining attention as the Korean government considers including COVID-19 vaccine to the National Immunization Program (NIP). The news presents a favorable opportunity for global pharmaceutical companies with vaccines. Consequently, these companies are focusing on publicizing the socioeconomic losses of COVID-19. According to the pharmaceutical industry on February 26, it was confirmed that the Korea Disease Control and Prevention Agency (KDCA) has begun research to evaluate the validity of COVID-19 vaccine inclusion to the NIP since last year and started the final review. Considering that the research began at the end of April last year, the result will likely be finalized in May. Based on the final result, it is possible that COVID-19 vaccines, along with influenza vaccines, will be included in the NIP in the second half. Therefore, the consideration for including in the NIP has brought attention the COVID-19 vaccine market. The global and Korean markets are dominated by Pfizer and Moderna. Recently, Moderna has been focusing on messaging the socioeconomic effects of the COVID-19 vaccine. Moderna Korea recently held the mRNA media insight event, announcing the importance of the COVID-19 vaccine. At the event, Dr. Hankil Lee of Ajou University Hospital College of Pharmacy, who presented "The Socioeconomic Impact of COVID-19 Losses and the Effects of Vaccination," noted that COVID-19 infections continue to cause significant socioeconomic damage. According to a Korean study (based on big data from the Health Insurance Review & Assessment Service) estimating productivity losses and medical expenses among the employed population, the societal losses attributable to COVID-19 reached approximately KRW 7 trillion in 2023. Specifically, among 25.16 million employed individuals aged 18 to 64, about 9.8 million sought outpatient care, roughly 140,000 required hospitalization, and 1,539 died. Based on these figures, the estimated direct medical costs amounted to approximately KRW 1.4 trillion, including KRW 540 billion for outpatient services, KRW 220 billion for inpatient treatment, and KRW 450 billion for post-illness care. Dr. Lee said, "It is the first study to estimate the national socioeconomic costs of COVID-19 infections using the latest domestic data sources," adding that "COVID-19 infections continue to impose a serious socioeconomic burden, and employee vaccination is evaluated as an effective strategy to reduce corporate losses and lower costs." Clinical settings have assessed that if COVID-19 vaccines are newly included in the NIP, they could help establish a new vaccine market. Inclusion in the NIP is deemed essential for stable market formation. Dr. Kwak Kyung-geun, President of the Seoul Physicians Association, stated, "In the case of COVID-19 vaccines, high-risk groups such as those aged 65 and older were supported by the government last year, and some COVID-19 vaccines were distributed privately. The procurement price was around KRW 100,000 per dose. I recall that not a single patient received the vaccine on a non-reimbursable basis, resulting in returns to the pharmaceutical companies." Dr. Kwak said, "If COVID-19 vaccines are included in the NIP, high-risk groups will be automatically covered, and, similar to influenza vaccines, the vaccination rate among these groups is expected to be high as the vaccine is perceived as essential," adding that "However, it is questionable whether relatively younger patients, excluding the high-risk groups, would choose to receive the vaccine on a non-reimbursable basis, despite potential global policy influences."
- Company
- Lunit presents AI breast cancer Dx results at ECR 2025
- by Whang, byung-woo Feb 28, 2025 05:58am
- On the 27th, Lunit, a medical artificial intelligence (AI) company, announced that it has presented 15 latest research achievements in the field of breast cancer diagnosis at the European Congress of Radiology 2025 (ECR 2025), which is being held in Vienna, Austria until the 2nd of next month. At the conference, Lunit presented 13 oral presentations and two poster presentations using the AI-based breast imaging analysis solution, Lunit INSIGHT MMG. In particular, it gained attention for presenting the clinical value of AI-based breast cancer diagnosis through collaborative research with prestigious European medical institutions. The most noted study presented by Lunit at ECR 2025 is a large-scale study conducted in collaboration with the Cancer Registry of Norway. The researchers analyzed more than 1 million mammography data from the Norwegian national breast cancer screening program (BreastScreen Norway) to explore whether Lunit Insight MMG could perform the role of one of two radiologists required for the current double reading system. The study found that when AI determined that there was a 10% or greater chance of breast cancer, it detected 79.9% of breast cancers found during actual screening, and when the chance of cancer was 5% or greater, it detected 75.5% of breast cancers found during actual screening. In particular, it demonstrated the effectiveness in early detection by finding an additional 5.7% of interval cancers that were missed during existing screenings. This proved empirically that the introduction of AI can significantly reduce the workload of specialists while maintaining the cancer detection rate. In addition, Lunit has collaborated with researchers at the Norwegian Institute of Public Health to evaluate the ability of AI to detect cancer at an early stage by applying Lunit Insight MMG to mammography data from more than 116,000 women who participated in the Norwegian National Breast Cancer Screening Program from 2004 to 2018. As a result, the AI detected the risk of future cancer six years before the final diagnosis. In addition, the AI analyzed cases of breast cancer detected during the screening process, and the cancer risk score increased significantly from 19.2 to 82.7, identifying lesions suspected of being breast cancer with high accuracy. On the other hand, women who did not have cancer maintained a consistently low AI risk score, and AI also smoothly detected an early risk increase in interval cancer. “The research presented at ECR 2025 once again demonstrated the high reliability and stability of Lunit's AI solutions,” said Beomseok Brandon Suh, CEO of Lunit. ”It is especially significant in that it has presented solutions to 2 key challenges: solving the shortage of specialists and early diagnosis.”
- Company
- Will patients taking osteoporosis drugs increase?
- by Moon, sung-ho Feb 28, 2025 05:58am
- With a denosumab biosimilar expected to enter the clinical trial site in Korea in earnest, changes in the treatment market are expected. # According to industry sources on the 24th, the Ministry of Health and Welfare recently announced a preliminary administrative notice of the revision of the 'Detailed Standards and Methods for the Application of Medical Benefits' centered on the listing of the denosumab biosimilar. Unless there is a major disagreement, the revision is likely to take effect next month. The item that will be listed is the Celltrion biosimilar ‘Stoboclo prefilled syringe (hereinafter referred to as Stoboclo).’ The drug is a biosimilar version of Amgen’s Prolia that has achieved unrivaled sales in the domestic osteoporosis treatment market, and the drug is expected to compete with the original product starting next month. The Ministry of Health and Welfare plans to revise the notice to apply the same reimbursement standards as Prolia. With the notice, interest is shifting to how Stoboclo’s reimbursment listing will spark competition with the original Prolia. The industry is interested in whether Stoboclo will be able to exert its influence as a biosimilar in the domestic market, as it has in the global market. Currently, the price of Prolia is KRW 154,700 per 60 mg. Stoboclo’s price is expected to be lower than this because it is a biosimilar. For reference, the Ministry of Health and Welfare expanded the reimbursement standard for osteoporosis treatment last year. It made it possible to continue applying the reimbursement to patients who have reached the treatment goal of the T-score, which is the standard for osteoporosis treatment and covered those on the borderline. When measuring bone density using dual-energy X-ray absorptiometry (DXA), the T-score is -2.5 or less (T-score ≤ -2.5), and the patient is approved for reimbursement, the patient is approved for reimbursement for an additional year even if the T-score improves to -2.5 or more and -2.0 or less during treatment. If the T-score is above -2.5 and below -2.0 even after treatment, the drug will be granted reimbursement for an additional year. The HIRA has been conducting selective intensive reviews since last year in anticipation of an increase in claims due to the expansion of reimbursement. The biosimilar Stoboclo will also be subject to these reimbursement standards, as will Prolia. The Ministry of Health and Welfare explained, “As Stoboclo is scheduled to be newly listed, it will be applied reimbursement standards in the same way as existing denosumab injection’s standard, and ‘etc.’ has been added to the product name in the notification category.” A professor of rheumatology at a tertiary hospital in Seoul said, “Previous osteoporosis drugs had to be taken on an empty stomach in the early morning and required sitting for a long time due to concerns about esophagitis.” He said, “The dosing method was that difficult to take.” He went on to say, “The treatment paradigm has changed significantly after the introduction of Prolia from the patient's perspective, as it provides injections like vaccinations. This has rapidly restructured the osteoporosis treatment market restructuring,” and expanded the market to expand further.
- Company
- Will the SC injection be a new treatment option for IBD?
- by Son, Hyung Min Feb 28, 2025 05:58am
- The clinical accomplishments of subcutaneous formulation (SC) new drugs are being noticed in the inflammatory bowel diseases (IBD) area, including Crohn's disease and ulcerative colitis. Celltrion's Remsima SC clinical results have recently shown improved endoscopic and histologic remission rates. Janssen's Tremfya SC induction therapy also showed results similar to the intravenous (IV) formulation. Remsima SC showed clinical recapture after dose escalation According to industry sources on February 27, Celltrion unveiled its clinical results during the European Crohn´s and Colitis Organisation (ECCO) annual conference held for four days in Berlin, Germany. Remsima SC is Celltrion's in-house developed biologic medicine, changing the existing IV injection to SC formulation. Remsima is a biosimilar version of Janssen's inflammatory bowel disease medication Remicade. In November 2019, Celltrion obtained approval for Remicade's SC injection formulation, Remsima, in Europe and began challenging the market. IBD is characterized by repetitive improvement and recurring chronic inflammation in the gastrointestinal tract caused by an abnormal immune response. Ulcerative colitis and Crohn's disease are types of IBD. Repetitive gastrointestinal tract symptoms, including diarrhea, blood in stool, and abdominal pain, significantly affect daily life but treatments are lacking. Therefore, patients need new treatments. CelltrionThe recently presented phase 3 clinical trial is a study result of Remsima SC involving patients with moderate to severe ulcerative colitis (UC) and Crohn's disease (CD). The analysis was based on two years of post hoc data analysis of the LIBERTY-CD and LIBERTY-UC clinical trials, which were the basis of approval. The effects were analyzed in patients who had a loss of response during the previous treatment with Remsima SC 120 mg, and then the dose was escalated to 240 mg. The analysis results indicate that 66.0% (31/47 patients) of the CD patients and 69.4% (43/62 patients) of UC patients showed clinical recapture after dose escalation following loss of response. Ultimately, 85.1% (40/47 patients) of CD patients and 82.3% (51/62 patients) of UC patients had clinical recapture at 102 weeks. Notably, in CD patients, the early clinical recapture group had increased serum drug levels from 8.0 to 22.1 μg/mL following dose escalation, and the later clinical recapture group had increased serum levels from 11.1 to 19.8μg/mL. In UC patients, both the early clinical recapture group and later clinical response group (7.4 to 16.5 μg/mL) had increased serum drug levels. A researcher said, "The current study result confirmed that dose escalation of Remsima SC induces rapid clinical recapture in patients who experienced loss of response. Through further studies, we need to analyze factors related to the clinical recapture rate in depth. Janssen's Tremfya SC induction therapy demonstrated effectiveness Janssen unveiled its clinical results for the SC formulation of Tremfya SC at ECCO 2025. Tremfya is an autoimmune disease therapy that blocks or inhibits the interleukin (IL)-23 signaling pathway. By suppressing IL-23, a key mediator of inflammation, the treatment has shown to be effective in several chronic immune-mediated conditions, including CD, UC, psoriasis, and palmoplantar pustulosis. JanssenThe efficacy of Tremfya was previously demonstrated in the QUASAR study using an IV induction therapy followed by SC maintenance therapy. In the recent Phase 3 ASTRO trial, the effectiveness and safety of SC induction therapy were evaluated in patients with moderate-to-severe UC. Treatment for IBD is divided into induction therapy and maintenance therapy. Induction therapy aims to induce remission in patients with severe active disease. Maintenance therapy is used to sustain remission. The ASTRO study was a multinational, randomized, double-blind, placebo-controlled trial that enrolled 418 UC patients who were either unresponsive or intolerant to corticosteroids, immunosuppressants, biological agents, or Janus kinase (JAK) inhibitors or who had not previously received these treatments. The primary endpoint was clinical remission at week 12, based on clinical indices and endoscopic scores. The clinical results revealed that the Tremfya SC group achieved a clinical remission rate of 27.6%, compared with 6.5% in the placebo group. Additionally, the endoscopic and histo-endoscopic mucosal improvement rates were 37.3% and 30.5% in the Tremfya SC group, which were substantially higher than the 12.9% and 10.8% observed in the placebo group. Safety profiles were comparable between the Tremfya SC and placebo groups, with similar incidences of adverse events (AEs), serious adverse events (SAEs), and AEs leading to treatment discontinuation. A researcher commented, "The ASTRO study provides important data that extends the previous Tremfya IV induction regimen results. This demonstrates that Tremfya is highly effective not only in its IV formulation but also in SC induction therapy, and it can be used in patients with moderate-to-severe UC without raising new safety concerns." Based on these clinical results, Janssen submitted a biologics license application (BLA) for Tremfya SC induction therapy to the U.S. Food and Drug Administration (FDA) in November last year.
- Company
- Will MSD’s rare cancer drug Welireg be reimbursed this time
- by Eo, Yun-Ho Feb 28, 2025 05:57am
- Attention is gathering as to whether the rare anticancer drug Welireg will succeed in its second attempt at reimbursement listing in Korea. According to industry sources, MSD Korea’s oral hypoxia-inducible factor-2 alpha (HIF-2α) inhibitor Welireg (belzutifan) will be presented to the Health Insurance Review and Assessment Service’s Cancer Disease Deliberation Committee in March this year. This drug was submitted for reimbursement in April last year and was put up for public petition in May, gaining the consent of more than 50,000 people, but it failed to overcome the CDDC review hurdle. The key to Welireg’s second reimbursement attempt will again be finances. Welireg was designated an orphan drug in Korea for the treatment of Von Hippel-Lindau disease in January last year, then formally approved in May of the same year. Specifically, the drug is indicated for the treatment of adult patients with VHL who require therapy for associated renal cell carcinoma (RCC), CNS hemangioblastoma, or pancreatic neuroendocrine tumors (pNET), that do not require immediate surgery. As a HIF-2α inhibitor, Welireg reduces transcription and expression of HIF-2α target genes associated with cellular proliferation, angiogenesis, and tumor growth. The drug’s efficacy was demonstrated in the open-label Study 004 trial, which investigated 61 patients with VHL-associated RCC who were diagnosed with at least one measurable solid tumor localized to the kidney. Patients enrolled in the trial had other VHL-associated tumors including CNS hemangioblastomas and pNET. The major efficacy endpoint of the clinical trial was the overall response rate (ORR) in patients with VHL-associated RCC as measured by radiology assessment using RECIST v1.1 as assessed by an independent review committee (IRC). Additional efficacy endpoints included duration of response (DoR) and time to response (TTR). In the study, Welireg showed an ORR of 49% in patients with VHL-associated RCC. All responses were partial responses. The median DoR had not yet been reached, and the DoR among responders who were still responding after at least 12 months was 56%. Median TTR was 8 months. Also, in patients with VHL-associated CNS hemangioblastomas, Welireg showed an ORR of 63%, with a complete response rate of 4% and a partial response rate of 58%. Recently, Welireg was additionally approved for a kidney cancer indication in the US. Its efficacy for the indication was confirmed in LITESPARK-005, a trial conducted on patients with unresectable locally advanced or metastatic clear cell renal cell carcinoma (RCC) that had progressed following both a PD-1 or PD-L1 checkpoint inhibitor and a VEGF-TKI. Results showed that Welireg improved progression-free survival (PFS) and reduced the risk of disease progression or death by 25% compared to everolimus in patients with advanced renal cell carcinoma who received a PD-1 or PD-L1 immune checkpoint inhibitor and a VEGF receptor-targeted therapy, either sequentially or in combination.
- Company
- Domestic approval application filed for 'Voranigo' in KOR
- by Eo, Yun-Ho Feb 27, 2025 05:57am
- Product photo of Voranigo New drug 'Voranigo' for malignant brain tumors has entered domestic approval procedure. According to the industry sources, Servier Korea has recently submitted approval application to the Ministry of Food and Drug Safety (MFDS) for Voranigo (vorasidenib). In Sepetember last year, this drug was designated an orphan drug in South Korea. Voranigo is indicated for the treatment of diffuse gliomas with an isocitrate dehydrogenase (IDH) mutation. Voranigo targets patients with low-grade gliomas who are vulnerable to IDH1 or IDH2 mutations. This drug is a bispecific inhibitor of IDH1/2, developed by multinational pharmaceutical company Servier. It targets glioma (astrocytoma or oligodendroglioma), a type of brain tumor that is difficult to treat. Voranigo received the final approval from the U.S. Food and Drug Administration (FDA) in August 2024 and is in the process of getting approved in countries worldwide, including Europe. The efficacy of Voranigo was demonstrated through the Phase 3 INDIGO study. The study results were presented at last year's American Society of Clinical Oncology (ASCO) Annual Meeting. The study results showed that in patients with glioma who have IDH mutation, the drug significantly reduced the tumor progression or death risk by 61% compared to the placebo. Voranigo also reduced the risk of requiring further treatments by 74%. The study participants had no history of undergoing treatments other than surgery. Voranigo also showed favorable drug tolerance. Its safety profile was similar to the Phase 1 clinical trial case results. Meanwhile, glioma is the most common type of primary malignant brain tumor in adults, and almost all adult patients (grade 2 diffuse gliomas) are likely to have IDH1 or IDH2 mutation. These patients are currently treated with off-label (medicines approved for other uses) instead of officially approved medicines. In addition to Voranigo monotherapy, Servier is currently conducting clinical trials for concurrent use of the drug with MSD's immune checkpoint inhibitor, 'Keytruda (ingredient: pembrolizumab),' in patients with relapsed and advanced gliomas who have IDH1 mutation. The company already has 'Tibsovo (IDH1 inhibitor)' and a 'IDH2 inhibitor' in its IDH inhibitor pipeline.
- Company
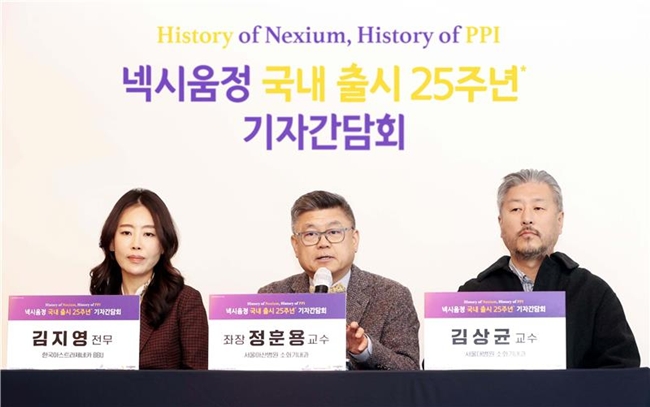
- Nexium challenged by P-CAB…attempts at regaining sales
- by Whang, byung-woo Feb 27, 2025 05:57am
- Proton pump inhibitors (PPIs) are being challenged by emerging P-CAB drugs. Therefore, Nexium's company is strengthening strategic partnerships to maintain Nexium's market position. The company continues partnering with Ildong Pharmaceutical and plans to continue collaboration based on its years of prescription experience. (from left) Ji-Young Kim, executive director of AstraZeneca Korea, Hwoon-Yong Jung, Professor in the Department of Gastroenterology at Asan Medical Center in Seoul, and Sang Gyun Kim, Professor in the Department of Gastroenterology at Seoul National University Hospital. AstraZeneca Korea announced this on February 20 at the press conference celebrating its 25-year anniversary of the South Korea launch of gastroesophageal reflux disease (GERD) treatment Nexium (esomeprazole magnesium trihydrate). Launched in 2000, Nexium is one of the major PPI treatments that works by suppressing gastric acid secretion. It has six indications, including GERD, and has the most indications among domestically approved PPIs. After 25 years since the launch of this drug, the effects on superior acid control and the improvement of GERD, as well as the effectiveness and safety profile of long-term administration, have been confirmed through various clinical practices. Nexium has been recorded as No.1 in accumulative prescription volume for 10 years in the global GERD treatment market, including PPI and P-CAB. Dr. Hwoon-Yong Jung, Professor in the Department of Gastroenterology at Asan Medical Center in Seoul, said, "Nexium is a s-isomer-based PPI with a superior treatment rate in 98.9% of patients with GERD. It has established a firm position in the market." Dr. Jung added, "It secured various indications, including maintenance therapy following intravenous injection to prevent rebleeding related to gastric ulcer. It is now known to provide a wide variety of treatment options." However, as the growth rate of PPI monotherapy has been decreasing, the company has deep concerns. According to market research firm UBIST, last year's outpatient prescription sales in the PPI monotherapy market were KRW 636.2 billion. The PPI monotherapy market steeply rose until 2021. After that, the growth rate significantly decreased. The prescription sales of PPI monotherapy in 2019 were KRW 461.7 billion and then increased by 19% to KRW 550.1 billion the following year. In 2021, the sales increased by 9% to KRW 600.4 billion. In 2022, the sales increased by only 2%, with KRW 614.3 billion. In 2023, it increased by 2% with KRW 624.5 billion. Last year, it rose by 2% compared to the previous year. After 2022, it grew 2% in three consecutive years. Analysis suggests that the introduction of P-CAB drugs has contributed to this sales trend. P-CAB drugs have a longer duration of drug action compared to PPI drugs, so they are also effective for managing night-time gastric acid secretion. They also have the advantage of combining with other medications because it is less likely to interact with other drugs. The total prescription sales of P-CAB drugs show a high growth rate: ▲2019, KRW 30.4 billion▲2020, KRW 77.1 billion ▲2021, KRW 110. 7 billion ▲2022, KRW 146.3 billion ▲2023, KRW 217.2 billion ▲2024, KRW 286.4 billion. Despite defending the market position, Nexium is seeing decreasing sales. The recent sales of Nexium indicate that its sales have been decreasing after recording the highest sales in 2020, with KRW 45.6 billion: ▲2021, KRW 42.0 billion ▲2022, KRW 33.5 billion ▲2023, KRW 32.3 billion ▲2024, KRW 29.1 billion. Despite this trend, experts view that Nexium will maintain its market position. Apart from the P-CAB drugs' effect, the long-term trend can be closely watched. Dr. Jung said, "New drug releases attract attention and can lead to increased usage, but existing drugs still have advantages and remain in use." Dr. Jung added, "P-CAB development has provided an additional treatment option that can enhance drug action in patients who are experiencing a decrease in the drug effectiveness." Dr. Sang Gyun Kim, Professor in the Department of Gastroenterology at Seoul National University Hospital, said, "The degree of symptom improvement experienced by patients are not significantly different between PPI and P-CAB. If a disease is effectively managed by PPI, there is no need to change the medication." Dr. Kim added. "We have to wait to see which medication will benefit patients more. Given that P-CAB has not been in the market for so long, we still need to monitor its long-term usage." Bae Yong-Chan, Executive Director of Ildong Pharmaceutical Along with this, AstraZeneca and Ildong Pharmaceutical plan to maintain their influence on the market by strengthening their partnership. Bae Yong-Chan, Executive Director of Ildong Pharmaceutical's ETC division, said, "Besides the gastroenterology area, we are strengthening partnerships to pave the way for cardiovascular diseases area. Also, Nexium's long-term maintenance therapy will still be its advantage." Bae added, "Nexium is a trusted medication that has contributed to improving patient quality of life. Ildong Pharmaceutical, in collaboration with AstraZeneca, is expanding Nexium's value. We will strive to create the best treatment settings through continued collaboration."